Summary
Abstract
Asthma guidelines recommend an inhaled corticosteroid plus a long-acting inhaled β2-agonist (β2-adrenoceptor agonist) as the preferred maintenance therapy for moderate and severe persistent asthma. Advair®/Seretide® Diskus®, also registered as Accuhaler®, is fixed-dose salmeterol (a long-acting inhaled β2-agonist) and fluticasone propionate (a corticosteroid) administered via a single powder inhalation device.
The clinical effectiveness of salmeterol/fluticasone propionate in patients with persistent asthma symptoms has been established in comparative clinical trials. Pharmacoeconomic analyses, based on data from these clinical trials, have been conducted from a healthcare payer perspective in various countries. In patients with asthma not controlled with inhaled corticosteroids, salmeterol/fluticasone propionate was associated with more favourable (lower) cost-effectiveness ratios than fluticasone propionate monotherapy, oral montelukast plus inhaled fluticasone propionate, inhaled budesonide, and inhaled formoterol plus budesonide. As the initial maintenance therapy in patients with persistent asthma symptoms while receiving short-acting β2-agonists alone, salmeterol/fluticasone propionate was cost effective relative to montelukast monotherapy. Although the total cost of asthma management tended to be slightly higher with salmeterol/fluticasone propionate than with fluticasone propionate or montelukast monotherapy, salmeterol/fluticasone propionate consistently had a more favourable cost-effectiveness ratio in terms of per successfully treated week or symptom-free day and/or was associated with small incremental costs to achieve significant additional clinical benefits. In clinical practice, salmeterol plus fluticasone propionate was associated with lower asthma-related costs than treatment with other maintenance therapies.
In patients with asthma symptoms despite treatment with inhaled corticosteroids, salmeterol/fluticasone propionate produced clinically meaningful improvements in overall Asthma Quality of Life Questionnaire (AQLQ) scores relative to salmeterol or placebo monotherapy, in emotional function domain scores relative to fluticasone propionate or budesonide, and in asthma symptoms domain scores relative to budesonide. In patients with persistent asthma symptoms while receiving short-acting β2-agonists alone, salmeterol/fluticasone propionate produced clinically meaningful improvements in overall AQLQ scores compared with fluticasone propionate or montelukast.
Conclusions: Pharmacoeconomic analyses indicate that salmeterol/fluticasone propionate administered via a single inhaler represents a cost-effective treatment option (relative to fluticasone propionate at the same nominal dosage, budesonide, formoterol plus budesonide and montelukast plus fluticasone propionate) in patients with asthma not controlled with inhaled corticosteroid therapy. In patients with asthma not controlled with short-acting β2-agonists alone, salmeterol/fluticasone propionate is a cost effective treatment relative to monotherapy with montelukast. Importantly, salmeterol/fluticasone propionate is also associated with improvements in health-related quality of life.
Asthma
Asthma, a chronic inflammatory disease of the airways, is among the most common chronic diseases worldwide and is increasing in prevalence. Among affected adults, lung function declines over time to a greater extent, and mortality rates are somewhat higher, than in individuals without asthma.
Asthma places a considerable economic burden on affected individuals and society at large. Healthcare costs are approximately twice as high in patients with asthma than in similar patients without asthma. Prescription medications and hospitalisation are the largest contributors to direct healthcare costs; loss of work is the largest contributor to indirect healthcare costs.
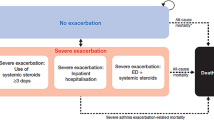
The cost of treating asthma increases if the underlying disease is severe or poorly controlled. Exacerbations, which result from poor control, may require costly physician and emergency room visits and hospitalisation. The use of appropriate maintenance therapy, although initially increasing drug and physician-based costs, may subsequently reduce direct healthcare costs and indirect costs by improving asthma control.
The symptoms of asthma can impair the individual’s health-related QOL (HR-QOL), and many physical activities, along with emotional and social aspects of a patient’s life, may be limited by the disease.
A stepwise approach to treatment based on the underlying severity of asthma symptoms is recommended in recent global asthma treatment guidelines to control symptoms and maintain normal activity levels. Use of an inhaled corticosteroid plus a long-acting inhaled β2-agonist β2-adrenoceptor agonist) is the preferred controller therapy in patients with moderate and severe persistent asthma.
Clinical Profile of Inhaled Salmeterol/Fluticasone Propionate
The long-acting inhaled β2-agonist salmeterol and the corticosteroid fluticasone propionate are administered in a single powder Diskus® (Accuhaler®) inhalation device, hereafter referred to as salmeterol/fluticasone propionate. The combination appears to have complementary effects and targets both smooth muscle dysfunction and inflammation.
In randomised, double-blind, comparator-controlled, multicentre trials in patients with asthma that were used as the basis for pharmacoeconomic analyses, salmeterol/fluticasone propionate was at least as effective clinically as other combination asthma treatments.
Salmeterol/fluticasone propionate twice daily for 12 weeks was more effective in improving most measures of lung function and asthma symptom outcomes than monotherapy twice daily with its individual components at the same nominal dosage in patients with asthma symptoms despite existing treatment with inhaled corticosteroids, salmeterol or short-acting β2-agonists alone.
Salmeterol/fluticasone propionate 50/100 or 50/250μg twice daily was significantly more effective in improving morning peak expiratory flow than monotherapy with budesonide 400 or 800μg twice daily, and at least as effective as the long-acting inhaled β2-agonist formoterol 12μg plus budesonide 800μg twice daily administered via separate inhalers, in 12- or 24-week studies in patients with moderate-to-severe asthma not controlled with inhaled corticosteroids.
In 12-week clinical trials in patients with asthma despite previous treatment with inhaled corticosteroids or short-acting β2-agonists alone, salmeterol/fluticasone propionate 50/100μg twice daily was significantly more effective in improving lung function and increasing the number of asthma-free days than the leukotriene modifier montelukast 10 mg/day alone or in combination with inhaled fluticasone propionate 100μg twice daily. In patients with persistent asthma symptoms while receiving short-acting inhaled β2-agonists alone, salmeterol/fluticasone propionate also demonstrated greater improvements than montelukast in the proportion of symptom- and rescue β2-agonist-free days, and nights with no awakenings.
Salmeterol/fluticasone propionate 50/100μg twice daily was more effective than inhaled beclomethasone 1000μg twice daily as a step-down therapy after treatment with high-dose corticosteroids in a small trial.
In clinical practice, salmeterol/fluticasone propionate improved asthma control (as assessed by the frequency of prescription refills for short-acting inhaled β2-agonists in retrospective studies) and compliance relative to other asthma maintenance treatments.
The type and severity of adverse events associated with each component drug may be expected in patients receiving salmeterol/fluticasone propionate in a single inhaler. Headache, throat irritation, hoarseness and candidiasis were the most frequent (incidence of each ≤4%) drug-related adverse effects associated with salmeterol/fluticasone propionate. The majority of the adverse events were mild to moderate in severity.
Pharmacoeconomic Analyses of Salmeterol/Fluticasone Propionate
Several cost-effectiveness analyses have been conducted on salmeterol/fluticasone propionate from the perspective of a healthcare payer in various countries; many of these results are currently available only in the form of abstracts. These analyses incorporated key clinical effectiveness and, in most analyses, prospective resource-use data from 12- or 24-week randomised, double-blind clinical studies of salmeterol/fluticasone propionate versus other asthma therapies. Each economic analysis included only direct healthcare costs (e.g. those associated with drug acquisition, rescue medication, unscheduled resource utilisation related to asthma exacerbation or treatment-related adverse events) of asthma using costs specific to the country of the analysis.
Salmeterol/fluticasone propionate 50/100, 50/250 and 50/500μg twice daily was clinically more effective than the same nominal dosage of fluticasone propionate twice daily in patients with asthma symptoms despite receiving treatment with inhaled corticosteroids. In three separate Swedish cost-effectiveness analyses, salmeterol/fluticasone propionate 50/100, 50/250 and 50/500μg had more favourable (lower) cost-effectiveness ratios than the corresponding dosage of fluticasone propionate. In a UK analysis based on a Markov model, salmeterol/fluticasone propionate 50/100μg had a mean incremental cost of each additional successfully controlled week of £20.83 per week (2000 values) relative to fluticasone propionate 100μg, and a 1.4-fold higher proportion of successfully controlled weeks per patient. In a probabilistic sensitivity analysis, salmeterol/fluticasone propionate was the dominant (more effective and less costly) strategy in 25% of cases. If decision makers are willing to pay approximately £45 for an additional successfully controlled week, salmeterol/fluticasone propionate will be the more cost-effective strategy in this patient population for 80% of the time.
Treatment with salmeterol/fluticasone propionate was less costly than treatment with budesonide or formoterol plus budesonide in patients with asthma not controlled with previous corticosteroid therapy in separate analyses. In pharmacoeconomic analyses in Sweden, Germany, Singapore and the UK, salmeterol/fluticasone propionate 50/100 or 50/250μg twice daily was associated with more effective treatment and lower asthma management costs than budesonide 400 or 800μg twice daily. Although clinical efficacy outcomes were similar between salmeterol/fluticasone 50/250μg twice daily and formoterol/budesonide 12/400μg twice daily administered via a single inhalation device, salmeterol/fluticasone propionate was less costly in pharmacoeconomic analyses that used a Markov model in Spain, Sweden and the UK. Similarly, in cost minimisation analyses in Australia, Canada, Norway, Spain and the UK, the total daily treatment costs with salmeterol/fluticasone propionate 50/250μg were approximately 16–46% lower than with formoterol 12μg plus budesonide 800μg.
Separate analyses have shown that salmeterol/fluticasone propionate 50/100μg twice daily was more cost effective than montelukast 10 mg/day with or without concurrent fluticasone propionate 100μg twice daily in patients with asthma. Although higher costs were associated with salmeterol/fluticasone propionate treatment than with montelukast monotherapy, cost-effectiveness ratios were more favourable (lower cost per outcome) with salmeterol/fluticasone propionate as the initial maintenance therapy in patients with persistent asthma not controlled with short-acting β2-agonists alone in US analyses. Compared with montelukast monotherapy, salmeterol/fluticasone propionate costs an extra $US0.46–1.33/day for each additional successfully treated patient, and an extra $US0.73–1.69/day for an additional symptom-free day (year of costing 2001 or not reported). Sensitivity analyses did not change the overall inferences, indicating that the results were robust to assumptions used in the economic analyses. In an analysis in The Netherlands, salmeterol/fluticasone propionate was more effective and less costly per week than montelukast plus fluticasone propionate in patients with asthma symptoms despite previous therapy with inhaled corticosteroids.
These pharmacoeconomic analyses are limited by the difficulty in predicting long-term treatment effects from data from short-term clinical trials (e.g. clinical trials may not capture all asthma- and drug-related adverse events and healthcare utilisations, and the source population may differ from patients treated in the community). Other limitations of these analyses include the lack of sensitivity analysis results, the lack of a common outcome measure, and the inclusion of only direct healthcare costs.
From the perspective of the French healthcare payer in 2000, the introduction of salmeterol/fluticasone propionate for the management of persistent asthma would be cost effective and affordable according to a budget impact model. Assuming 100% treatment compliance, total annual cost savings of €2.7 million and €1.9 million would result if 100% of patients were switched to salmeterol/fluticasone propionate from salmeterol plus fluticasone propionate or from formoterol plus budesonide. These changes in treatment equate to an additional 4067 and 2939 patients receiving salmeterol/fluticasone propionate for the same budget.
In patients with asthma enrolled in US managed-care plans, treatment with salmeterol plus fluticasone propionate was less costly than treatment with an inhaled corticosteroid plus another maintenance medication (e.g. another inhaled corticosteroid plus salmeterol or an inhaled corticosteroid plus an oral leukotriene modifier) in retrospective studies that considered only direct healthcare costs.
QOL Assessments
The achievement of asthma control is related to improvements in HR-QOL. Overall and individual Asthma Quality of Life Questionnaire (AQLQ) domain scores (symptoms, emotional function, activity limitation and environmental stimuli) were assessed in some of the clinical trials of salmeterol/fluticasone propionate in patients with persistent asthma. A change ≥ 0.5 points in overall or domain scores is considered clinically meaningful.
Overall and individual AQLQ domain scores improved from baseline to a clinically meaningful extent with salmeterol/fluticasone 50/100 and 50/250€g twice daily in patients with asthma symptoms despite previous treatment with inhaled corticosteroids or short-acting β2-agonists alone.
In addition, in patients with asthma symptoms not controlled with short-acting β2-agonists alone, clinically meaningful and statistically significant improvements in overall AQLQ scores were shown with salmeterol/fluticasone propionate 50/100μg twice daily compared with monotherapy with fluticasone propionate 100μg twice daily or montelukast 10mg once daily. All between-group differences in individual AQLQ domain scores for salmeterol/fluticasone propionate versus montelukast were statistically significant and, with the exception of activity limitation in both trials and environmental exposure in one trial, clinically meaningful in favour of salmeterol/fluticasone propionate.
Moreover, in patients with asthma symptoms despite receiving inhaled corticosteroids, overall AQLQ scores improved by a statistically significantly greater extent with salmeterol/fluticasone propionate than with twice-daily monotherapy with its individual components, placebo or budesonide 800μg. Clinically meaningful changes from baseline in overall and AQLQ domain scores were shown with salmeterol/fluticasone propionate compared with salmeterol monotherapy or placebo, in emotional function compared with fluticasone propionate 100 or 250μg monotherapy, and in emotional function and asthma symptoms compared with budesonide.
The majority (68%) of 3603 patients with asthma in an observational study showed clinically meaningful improvements from baseline in overall AQLQ score after receiving salmeterol/fluticasone propionate 50/250μg twice daily for 8 weeks. According to this study, 1.5 patients needed to be treated with salmeterol/fluticasone propionate in order for one patient to demonstrate a ≥0.5 point improvement in AQLQ score.
As a corticosteroid step-down therapy, salmeterol/fluticasone maintained the improvements in HR-QOL achieved with high-dose inhaled corticosteroid therapy. In contrast, patients receiving beclomethasone 200μg twice daily lost some of these improvements.















Similar content being viewed by others
Notes
The use of tradenames is for product identification purposes only and does not imply endorsement.
References
Nelson HS. Advair: combination treatment with fluticasone propionate/salmeterol in the treatment of asthma. J Allergy Clin Immunol 2001; 107 (2): 397–416
Stoloff S, Poinsett-Holmes K, Dorinsky PM. Combination therapy with inhaled long-acting β2-agonists and inhaled corticosteroids: a paradigm shift in asthma management. Pharmacotherapy 2002 Feb; 22 (2): 212–26
Anderson GP. Interactions between corticosteroids and β-adrenergic agonists in asthma disease induction, progression, and exacerbation. Am J Respir Crit Care Med 2000; 161: S188–96
Barnes PJ. Scientific rationale for inhaled combination therapy with long-acting β2-agonists and corticosteroids. Fur Respir J 2002; 19: 182–91
Markham A, Jarvis B. Inhaled salmeterol/fluticasone propionate combination: a review of its use in persistent asthma. Drugs 2000 Nov; 60 (5): 1207–33
Markham A, Adkins JC. Inhaled salmeterol/fluticasone propionate combination: a pharmacoeconomic review of its use in the management of asthma. Pharmacoeconomics 2000 Dec; 18 (6): 591–608
Global strategy for asthma management and prevention. NHLBI/WHO workshop report (revised 2002). National Institutes of Health [online]. Available from URL: http://www.ginasthma.com [Accessed 2003 Mar 4]
Anon. Forecasted state-specific estimates of self-reported asthma prevalence: United States, 1998. MMWR Moth Mortal Wkly Rep 1998; 47: 1022–5
Sly RM. Changing prevalence of allergic rhinitis. Ann Allergy Asthma Immunol 1999 Mar; 82: 233–52
Grol MIL, Gerritsen J, Postma DS. Asthma: from childhood to adulthood. Allergy 1996; 51: 855–69
Lange R, Praner J, Vestbo J, et al. A 15-year follow-up study of ventilatory function in adults with asthma. N Engl J Med 1998 Oct 22; 339 (17): 1194–200
Lange P, Ulrik CS, Vestbo J, et al. Mortality in adults with self-reported asthma. Lancet 1996 May 11; 347: 1285–9
Reed CE. The natural history of asthma in adults: the problem of irreversibility. J Allergy Clin Immunol 1999 Apr; 103 (4): 539–47
Fuhlbrigge AL, Adams RJ, Guilbert TW, et al. The burden of asthma in the United States: level and distribution are dependent on interpretation of the National Asthma Education and Prevention Program Guidelines. Am J Respir Crit Care Med 2002; 166: 1044–9
Meng YY, Leung WM, Berkbigler D, et al. Compliance with US asthma management guidelines and specialty care: a regional variation or national concern? J Eval Clin Pract 1999; 5 (2): 213–21
Colice GL, Vanden Burgt J, Song J, et al. Categorizing asthma severity. Am J Respir Crit Care Med 1999; 160: 1962–7
National Institutes of Health. Highlights of the Expert Panel Report 2: guidelines for the diagnosis and management of asthma. Bethesda (MD): National Institutes of Health (National Heart, Lung, and Blood Institute), 1997 Jul. NIH publication no. 97-4051A
European Community Respiratory Health Survey. Variations in the prevalence of respiratory symptoms, self-reported asthma attacks, and the use of asthma medication in the European Community Respiratory Health Survey (ECRHS). Fur Respir J 1996; 9: 687–95
International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. Lancet 1998; 351: 1225–32
Chinn S, Burney P, Jarvis D, et al. Variation in bronchial responsiveness in the European Community Respiratory Health Survey (ECRHS). Fur Resp J 1997; 10: 2496–501
Hartert TV, Peebles Jr RS. Epidemiology of asthma: the year in review. Curr Opin Pulm Med 2000; 6: 4–9
Enright PL, McClelland RL, Newman AB, et al. Underdiagnosis and undertreatment of asthma in the elderly. Cardiovascular Health Study Research Group. Chest 1999; 116: 603–13
Armstrong EP, Krueger K, Langley PC. Analysis of asthma-related costs and patterns of resource utilization in a managed-care population. Dis Manage Health Outcomes 2001; 9 (3): 161–71
Peat JK. Changes in the prevalence of asthma and allergy in Australian children 1982–1992 [abstract]. Am Rev Respir Dis 1993; 147: A800
Peat JK, Haby M, Spijker J, et al. Prevalence of asthma in adults in Busselton, Western Australia. BMJ 1992; 305: 1326–9
Suissa S, Ernst P, Benayoun S, et al. Low-dose inhaled corticosteroids and the prevention of death from asthma. N Engl J Med 2000; 343: 332–6
Weissflog D. Epidemiology and costs of bronchial asthma and chronic bronchitis in Germany [abstract no. PRS17]. Value Health 2000 Sep-2000 31; 3: 333
Accordini S, Cazzoletti L, Gerzeli S, et al. The economic cost of current asthma in Italy: results of the Italian study on asthma in young adults (ISAYA) [abstract no. P2716]. Fur Respir J 2002 Sep; 20 Suppl. 38: 427s
Ungar WJ, Coyle PC. Prospective study of the patient-level cost of asthma care in children. Pediatr Pulmonol 2001 Aug; 32: 101–8
Birnbaum HG, Berger WE, Greenberg PE, et al. Direct and indirect costs of asthma to an employer. J Allergy Clin Immunol 2002 Feb; 109: 264–70
Cistemas MG, Blanc PD, Yen III, et al. Direct and indirect costs of adult asthma: a comprehensive study [abstract]. Chest 2002 Oct; 122 Suppl.: 1s
Jansson S-A, Jönsson E, Rönmark E, et al. Main cost drivers of costs for asthma in society-report from the obstructive lung disease in Northern Sweden studies [abstract no. P2959]. Fur Respir J 2001 Sep; 18 Suppl. 33: 441s
Wang SW, Liu X, Wiener DJ, et al. Comparison of prevalence, cost, and outcomes of a combination of salmeterol and fluticasone therapy to common asthma treatments. Am J Manag Care 2001 Sep; 7 (9): 913–22
Druss BG, Marcus SC, Olfson M, et al. Comparing the national economic burden of five chronic conditions: one-quarter of the U.S. population has one or more of these five chronic condi tions, which cost $62.3 billion in 1996. Health Aff (Millwood) 2001 Nov-2001 31; 20: 233–41
Pannicker S, Nielsen K, Martin BC. The net cost of asthma to a US public Medicaid program [abstract no. RP2]. Value Health 2001 Nov-2001 31; 4: 419
Grupp-Phelan J, Lozano P, Fishman P. Health care utilization and cost in children with asthma and selected comorbidities. J Asthma 2001; 38 (4): 363–73
Himmelberger DU, Antonicelli L. The relationship between resource consumption and asthma severity among asthmatic outpatients in three European countries [abstract no. 36]. Qual Life Res 2001; 10 (3): 201
Godard P, Chanez P, Siraudin L, et al. Costs of asthma are correlated with severity: a 1-yr prospective study. Fur Respir J 2002 Jan; 19: 61–7
Bratton DL, Price M, Gavin L, et al. Impact of a multidisciplinary day program on disease and healthcare costs in children and adolescents with severe asthma: a two-year follow-up study. Pediatr Pulmonol 2001 Mar; 31: 177–89
Van Ganse E, Laforest L, Pietri G, et al. Persistent asthma: disease control, resource utilisation and direct costs. Fur Respir J 2002 Aug; 20: 260–7
Korhonen K, Reijonen TM, Remes K, et al. Reasons for and costs of hospitalization for pediatric asthma: a prospective 1-year follow-up in a population-based setting. Pediatr Allergy Immunol 2001 Dec; 12: 331–8
Barnes PJ, Jonsson B, Klim JB. The costs of asthma. Fur Respir J 1996; 9: 636–42
Osman LM, McKenzie L, Cairns J, et al. Patient weighting of importance of asthma symptoms. Thorax 2001; 56: 138–42
Juniper EF. Using humanistic health outcomes data in asthma. Pharmacoeconomics 2001; 19 Suppl. 2: 13–9
Juniper EF, Guyatt GH, Ferrie PJ, et al. Measuring quality of life in asthma. Am Rev Respir Dis 1993; 147: 832–8
Bousquet J. Quality-of-life in allergic diseases. Rev Fr Allergol Immunol Clin 1998; 38 Suppl. 7S: S202–5
Rameckers E. Using health outcomes data to inform decisionmaking: patient perspective. Pharmacoeconomics 2001; 19 Suppl. 2: 53–5
Juniper EF, Guyatt GH, Epstein RS, et al. Evaluation of impairment of health related quality of life in asthma: development of a questionnaire for use in clinical trials. Thorax 1992; 47: 76–83
Rabe KF, Vermeire PA, Soriano JB, et al. Clinical management of asthma in 1999: the Asthma Insights and Reality in Europe (AIRE) study. Fur Respir J 2000; 16: 802–7
Lewis TC, Parker EA, Brakefield-Caldwell W, et al. Preliminary results of a community-based participatory research (CBPR) intervention to reduce exposure to household environ mental triggers of asthma [abstract no. B085]. 99th International Conference of the American Thoracic Society; 2003 May 16–21; Seattle, (abstracts-on-disk)
Bateman ED, Frith LF, Braunstein GL. Achieving guidelinebased asthma control: does the patient benefit? Fur Respir J 2002; 20 (3): 588–95
British Thoracic Society, Scottish Intercollegiate Guidelines Network. British guidelines on the management of asthma. Thorax 2003; 58 Suppl. 1: il–94
National Asthma Education and Prevention Program Expert Panel Report. Guidelines for the diagnosis and management of asthma-update on selected topics 2002 [online]. Available from URL: http://www.nhlbi.nih.gov/guidelines/asthma/ [Accessed 2003 Apr 9]
Piecoro LT, Potoski M, Talbert JC, et al. Asthma prevalence, cost, and adherence with expert guidelines on the utilization of health care services and costs in a state Medicaid population. Health Serv Res 2001 Jun; 36: 357–71
Nelson HS, Chapman KR, Pyke SD, et al. Enhanced synergy between fiuticasone propionate and salmeterol inhaled from a single inhaler versus separate inhalers. J Allergy Clin Immunol 2003 Jul; 112 (1): 29–36
Van den Berg NJ, Ossip MS, Hederos CA, et al. Salmeterol/ fiuticasone propionate (50/500 μg) in combination in a Diskus inhaler (Seretide) is effective and safe in children with asthma. Pediatr Pulmonol 2000; 30: 97–105
Bateman ED, Britton M, Carrillo J, et al. Salmeterol/fiuticasone combination inhaler: a new, effective and well tolerated treatment for asthma. Clin Drug Invest 1998 Sep; 16 (3): 193–201
Chapman KR, Ringdal N, Backer V, et al. Salmeterol and fiuticasone propionate (50/250 μg) administered via combination Diskus inhaler: as effective as when given via separate Diskus inhalers. Can Respir J 1999 Jan-1999 28; 6 (1): 45–51
Aubier M, Pieters WR, Schlösser NJJ, et al. Salmeterol/fluticasone propionate (50/500 μg) in combination in a Diskus inhaler (Seretide) is effective and safe in the treatment of steroid-dependent asthma. Respir Med 1999 Dec; 93: 876–84
Baraniuk IN, Ali M, Brody D, et al. Glucocorticosteroids induce β2-adrenergic receptor function in human nasal mucosa. Am J Respir Crit Care Med 1997; 155: 704–10
Mak JCW, Nishikawa M, Shirasaki H, et al. Protective effects of glucocorticoid on downregulation of pulmonary β2-adrenergic receptors in vivo. J Clin Invest 1995; 96: 99–106
Eickelberg O, Roth M, Lörx R, et al. Ligand-independent activation of the glucocorticoid receptor by β2-adrenergic receptor agonists in primary human lung fibroblasts and vascular smooth muscle cells. J Biol Chem 1999 Jan 8; 274 (2): 1005–10
Kavuru M, Melamed J, Gross G, et al. Salmeterol and fluticasone propionate combined in a new powder inhalation device for the treatment of asthma: a randomized, double-blind, placebo-controlled trial. J Allergy Clin Immunol 2000 Jun; 105 (Pt. 1): 1108–16
Shapiro G, Lumry W, Wolfe J, et al. Combined salmeterol 50 μg and fluticasone propionate 250 μg in the Diskus device for the treatment of asthma. Am J Respir Crit Care Med 2000 Feb; 161: 527–34
Rosenthal RR, Blake K, Strek M, et al. Fluticasone propionate/salmeterol Diskus combination product provides superior asthma control compared with fluticasone propionate and salme terol alone in patients previously receiving prn short-acting beta2-agonists alone [abstract no. 747]. J Allergy Clin Immunol 2002 Jan; 109 (1 Suppl.): 245
Jenkins C, Woolcock AJ, Saarelainen P, et al. Salmeterol/fluticasone propionate combination therapy 50/250 μg twice daily is more effective than budesonide 800 μg twice daily in treating moderate to severe asthma. Respir Med 2000 Jul; 94: 715–23
Johansson G, McIvor RA, D’Ambrosio FP, et al. Comparison of salmeterol/fluticasone propionate combination with budeso-nide in patients with mild-to-moderate asthma. Clin Drug Invest 2001; 21 (9): 633–42
Ringdal N, Chuchalin A, Chovan L, et al. Evaluation of different inhaled combination therapies (EDICT): a randomised, double-blind comparison of Seretide (50/250 μg bd Dis kus vs. formoterol (12 μg bd) and budesonide (800 μg bd) given concurrently (both via Turbuhaler) in patients with moderate-to-severe asthma. Respir Med 2002 Nov; 96 (11): 851–61
Calhoun WJ, Nelson HS, Nathan RA, et al. Comparison of fluticasone propionate-salmeterol combination therapy and montelukast in patients who are symptomatic on short acting β2-agonists alone. Am J Respir Crit Care Med 2001; 164: 759–63
Pearlman DS, White MV, Lieberman AK, et al. Fluticasone propionate/salmeterol combination compared with montelukast for the treatment of persistent asthma. Ann Allergy Asthma Immunol 2002 Feb; 88: 227–35
Nelson HS, Buss WW, Kerwin E, et al. Fluticasone propionate/salmeterol combination provides more effective asthma control than low-dose inhaled corticosteroid plus montelukast. J Allergy Clin Immunol 2000; 106: 1088–95
Ringdal N, Eliraz A, Pruzinec R, et al. The salmeterol/fluti-casone combination is more effective than fluticasone plus oral montelukast in asthma. Respir Med 2003 Mar; 97 (3): 234–41
Fowler SJ, Currie GP, Lipworth BJ. Step-down therapy with low-dose fluticasone-salmeterol combination or medium-dose hydrofluoroalkane 134x-beclomethasone alone. J Allergy Clin Immunol 2002 Jun; 109 (6): 929–35
Stempel D, Stanford RH, Murphy T, et al. Fluticasone propionate/salmeterol in a single inhaler improves refill persistence compared to fluticasone propionate and salmeterol from two separate inhalers [abstract no. A039]. 99th International Conference of the American Thoracic Society; 2003 May 16–21; Seattle, (abstracts-on-disk)
Carranza Rosenwieg JR, Stempel DA, Meyer J, et al. Improved compliance with fluticasone propionate and salmeterol in a single inhaler compared to other controller therapies [abstract no. C039]. 99th International Conference of the American Thoracic Society; 2003 May 16–21; Seattle, (abstracts-on-disk)
McCarthy TP, Rice L, Blair CA, et al. Improved compliance with asthma therapy in children treated with salmeterol/fluticasone propionate combination (SFC) compared with concur rent salmeterol (S) plus inhaled corticosteroid (ICS) or ICS alone [abstract no. C039]. 99th International Conference of the American Thoracic Society; 2003 May 16–21; Seattle, (abstracts-on-disk)
McCarthy TP, Rice L, Blair CA, et al. Improved asthma control achieved with salmeterol/fluticasone propionate combination (SFC) compared with concurrent inhaled long-acting β2-agonist (LAB) plus inhaled corticosteroid (ICS) therapy or ICS alone [abstract no. D034]. 99th International Conference of the American Thoracic Society; 2003 May 16–21; Seattle, (abstracts-on-disk)
McCarthy TP, Rice L, Blair CA. Salmeterol/fluticasone propionate combination (SFC) is associated with improved asthma control and compliance in children compared with concur rent salmeterol (S) plus inhaled corticosteroid (ICS) [abstract no. D034]. 99th International Conference of the American Thoracic Society; 2003 May 16–21; Seattle, (abstracts-on-disk)
Tews IT, Volmer T. Differences in compliance between combined salmeterol/fluticasone propionate (50/250μg) in the the Diskus device and fluticasone + salmeterol given via separate Diskus inhalers [abstract no. A59]. Am J Respir Crit Care Med 2002 Apr; 165 (8 Suppl Pt 2): A188. Plus poster presented at the 98th International Conference of the American Thoracic Society; 2002 May 17–22; Atlanta
Lanes SF, Garcia Rodriguez LA, Huerta C. Respiratory medications and risk of asthma death. Thorax 2002 Aug; 57 (8): 683–6
G1axoSmithKline. Seretide in asthma monograph [compact disk]. 3rd ed. G1axoSmithKline, 2003 Mar
GlaxoSmithKline. Advair Diskus 100/50, 250/50 and 500/50 prescribing information. Research Triangle Park (NC), 2002 Aug
Johansson G, Price MJ, Sondhi S. Cost-effectiveness analysis of salmeterol/fluticasone propionate 50/100μg vs fluticasone propionate 100μg in adults and adolescents with asthma. III: results. Pharmacoeconomics 1999; 16 Suppl. 2: 15–21
Palmqvist M, Price MJ, Sondi S. Cost-effectiveness analysis of salmeterol/fluticasone propionate 50/250μg vs fluticasone propionate 250μg in adults and adolescents with asthma. IV: results. Pharmacoeconomics 1999; 16 Suppl. 2: 23–8
Pieters WR, Lundback B, Sondi S, et al. Cost-effectiveness analysis of salmeterol/fluticasone propionate 50/500μg vs fluticasone propionate 500μg in adults and adolescents with asthma. V: results. Pharmacoeconomics 1999; 16 Suppl. 2: 29–34
Price MJ, Briggs AH. Development of an economic model to assess the cost effectiveness of asthma management strategies. Pharmacoeconomics 2002; 20 (3): 183–94
Becker I, Kielborn A, Price MJ, et al. Cost-effectiveness of salmeterol/fluticasone combination product and budesonide in asthma patients in Germany [abstract no. P854]. European Respiratory Society; 1999 Oct 9–13; Madrid, Spain, (abstracts-on-disk)
Chew FT, Lim TK, Lee BW, et al. Cost-effectiveness analyses comparing Seretide (salmeterol/fluticasone propionate combination product) and budesonide for the treatment of asthma in Singapore [abstract no. P3204]. Fur Respir J 2000 Aug; 16 Suppl. 31: 456s
Lundback B, Jenkins C, Price MJ, et al. Cost-effectiveness of salmeterol/fluticasone propionate combination product 50/250 μg twice daily and budesonide 800 μg twice daily in the treatment of adults and adolescents with asthma. Respir Med 2000 Jul; 94: 724–32
Pamaby A, Lloyd A, Browning D, et al. A comparison of the cost-effectiveness of salmeterol/fluticasone combination inhaler and budesonide in the management of asthma [abstract no. P156]. Thorax 2000 Dec; 55 Suppl. 3: A64
Price MJ, Briggs AH, Williams J. Development of an economic model to evaluate the cost-effectiveness of treatments in achieving asthma control [abstract]. Am J Respir Crit Care Med 2001 Apr; 163 (5 Suppl. Pt 2): A505
Rodriguez Barrios J, Sondi S. Economic evaluation of seretide vs budesonide/formoterol in Spain [abstract no. 190]. 9th Conference of the European Society of General Practice/Family Medicine; 2003 Jun 18–21; Ljubljana, Slovenia
Sondhi S, Martin A. Economic evaluation of salmeterol/fluticasone propionate combination versus budesonide/formoterol in the UK [abstract no. B106]. 99th International Conference of the American Thoracic Society; 2003 May 16–21; Seattle, (abstracts-on-disk)
Price MJ, Briggs AH. The cost-effectiveness of achieving asthma control with the combination products salmeterol/fluticasone propionate or formoterol/budesonide [abstract no. P1075. Fur Respir J 2001 Sep; 18 Suppl. 33: 159s
Jenkins C, Wilson J, Rutherford C, et al. Asthma management costs are lower with combination fluticasone/salmeterol (250/ 50 mcg bd) in a single inhaler than with budesonide 800 mcg bd plus eformoterol 12 mcg bd via separate inhalers [abstract no. P23]. Respirology 2002 Mar; 7 Suppl.: A20
Rance L, Musin A. Asthma management costs in Canada are lower with combination fluticasone propionate/salmeterol (250/50 mcg bid) in a single inhaler than with budesonide 800mcg bid plus eformoterol 12mcg bid via separate inhalers [abstract]. Chest 2002 Oct; 122 Suppl.: 2S–3S
Alonso JF, Badiola C, Kielhorn A. Economic evaluation of salmeterol/fluticasone combination vs budesonide plus formoterol in Spain [abstract no. P418]. Fur Respir J 2001 Sep; 18 Suppl. 33: 49s
Martin AA, Whitehead PJ, McCarthy TP. Asthma costs with salmeterol/fluticasone combination 50/250mcg bd compared to budesonide 800mcg plus formoterol 12mcg bd [abstract no. D034]. 99th International Conference of the American Thoracic Society; 2003 May 16–21; Seattle, (abstracts-on-disk)
Sheth K, Borker R, Emmett A, et al. Cost-effectiveness comparison of salmeterol/fluticasone propionate versus montelukast in the treatment of adults with persistent asthma. Pharmacoeconomics 2002; 20 (13): 909–18
Leibman C, Pathak D, Bowers B, et al. Cost-effectiveness analysis of fluticasone propionate/salmeterol combination versus montelukast in the treatment of adults with asthma [ab stract no. 549]. J Allergy Clin Immunol 2002 Jan; 109 Suppl.: S185
Stanford RH, Borker R, Dorinsky P, et al. The costs and efficacy of fluticasone propionate/salmeterol combination versus montelukast in the treatment of adults with persistent asthma [abstract]. Chest 2002 Oct; 122 Suppl.: 183S–4S
Leibman CW, Stanford R, Emmett A, et al. Cost-effectiveness of fluticasone propionate/salmeterol combination versus fluticasone + montelukast in the treatment of persistent asthma [abstract]. Am J Respir Crit Care Med 2002 Apr; 165 (8 Suppl. Pt 2): B4. Plus poster presented at the 98th International conference of the American Thoracic Society; 2002 May 17–22; Atlanta
Pieters WR, Wilson KK, Smith HCE, et al. Cost-effectiveness of fluticasone propionate/salmeterol combination product and fluticasone propionate/montelukast in asthma [abstract]. Am J Respir Crit Care Med 2001 Apr; 163 (5 Suppl. Pt 2): 643
Rutten-van Mölken MPMH, Van Doorslaer EKA, Jansen MCC, et al. Costs and effects of inhaled corticosteroids and bronchodilators in asthma and chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1995; 151: 975–82
Gold MR, Patrick DL, Torrance GW, et al. Identifying and valuing outcomes. In: Gold MR, Siegel JE, Russell LB, et al, editors. Cost-effectiveness in health and medicine. New York: Oxford University Press, 1996: 82–123
Kallmes DF, Kallmes MIL. Cost-effectiveness of angiography performed during surgery for ruptured intracranial aneurysms. Am J Neuroradiol 1997 Sep; 18: 1453–62
Hayman JA, Hillner BE, Harris JR, et al. Cost-effectiveness of adding an electron-beam boost to tangential radiation therapy in patients with negative margins after conservative surgery for early-stage breast cancer. J Clin Oncol 2002 Jan; 18 (2): 287–95
Continuing Medical Education (CME): Princeton Media Associate- healthcare and managed care courses. Pharmacoeconomics of lipid management [online]. Available from URL: http://www.prineetoneme.com/public/2001-01/reportl0.html [Accessed 2003 Aug 1]
Hoskins G, Smith B, Thomson C, et al. The cost implications of an asthma attack. Pediatr Asthma Allergy Immunol 1998; 12: 193–8
Stahl E, Borg S, Andersson F. Utility measures of severe and mild exacerbations reported by asthma patients [abstract no. 1087]. Fur Respir J 1999; 14 Suppl. 30: 148s
Lundbäck B, Pieters WR, Johansson G, et al. Cost-effectiveness analyses of salmeterol/fluticasone propionate combination product and fluticasone propionate in patients with asthma. I: introduction and overview. Pharmacoeconomics 1999; 16 Suppl. 2: 1–8
FXConverter - 164 Currency Converter [online]. Available from URL: http://www.onada.com/convert/classic [Accessed 2003 Jul 31]
Zetterström O, Buhl R, Mellem H, et al. Improved asthma control with budesonide/formoterol in a single inhaler, compared with budesonide alone. Fur Respir J 2001; 18: 262–8
Thomas M, Haughney J, Price D. Cost effectiveness of asthma management strategies [letter]. Pharmacoeconomics 2002; 20 (11): 789
Detoumay B, Pribil C, Jourdanne C, et al. Budget impact model for determining the costs of introducing inhaled salmeterol/ fluticasone propionate combination for the management of persistent asthma in France. Fur J Health Econom 2002; 3: 149–55
O’Connor RD, O’Donnell JC, Pinto LA, et al. Two-year retrospective economic evaluation of three dual-controller therapies used in the treatment of asthma. Chest 2002 Apr; 121 (4): 1028–35
Stempel DA, O’Donnell JC, Meyer JW. Inhaled corticosteroids plus salmeterol or montelukast: effects on resource utilization and costs. J Allergy Clin Immunol 2002 Mar; 109: 433–9
Krishnan AA, O’Connor RD, Bowers B, et al. Economic impact of treatment options in management of asthma [abstract]. Am J Respir Crit Care Med 2002; 165 (8 Suppl. Pt 2): A45
Juniper EF, Guyatt GH, Willan A, et al. Determining a minimal important change in a disease-specific quality of life questionnaire. J Clin Epidemiol 1994; 47 (1): 88–7
Juniper EF, Jenkins C, Price MJ, et al. Impact of inhaled salmeterol/fluticasone propionate combination product versus budesonide on the health-related quality of life of patients with asthma. Am J Respir Med 2002; 1 (6): 435–40
Reese PR, Mahajan P, Woodring A. Salmeterol/fluticasone propionate combination improves quality of life in asthma patients [abstract no. P0325]. Fur Respir 1998 Sep; 12 Suppl. 28: 35s
McCarthy TP, Edin HM, House K, et al. The effects of salmeterol/fluticasone combination (SFC) dry powder inhaler (DPI) on asthma control and quality of life, in patients pre viously treated with inhaled corticosteroids (ICS) [abstract no. P58]. Thorax 2001 Dec; 56 Suppl. 3: 63–64
Davis EA, Bowers B, Pepsin P, et al. The impact of fluticasone propionate/salmeterol combination product compared to oral montelukast on asthma related quality of life [abstract]. Am J Respir Crit Care Med 2001 Apr; 163 (5 Suppl. Pt 2): A506
Edin HM, Lang ML, Vandermeer AK, et al. Fluticasone propionate/salmeterol Diskus combination product improves asthma-related quality of life compared with individual compon ents in asthma patients symptomatic on (32 agonists alone [abstract no. 733]. J Allergy Clin Immunol 2002 Jan; 109 Suppl.: S241. Plus poster presented at the 58th Annual Meeting of the American Academy of Allergy, Asthma and Immunology; 2002 Mar 1–6; New York City
Edin HM, Prillaman B, Baitinger LA, et al. Improved ability to perform strenuous activities after treatment with fluticasone propionate/salmeterol combination [abstract]. Am J Respir Crit Care Med 2002 Apr; 165 (8 Suppl. Pt 2): A112
Tews IT, Trautmann M, Meyer A. The impact of salmeterol/fluticasone propionate combination product on asthma related quality of life [abstract no. 3489]. Fur Respir 2001 Sep; 18 Suppl. 33: 517s–8s
Zillich AJ, Blumenschein K, Johannesson M, et al. Assessment of the relationship between measures of disease severity, quality of life, and willingness to pay in asthma. Pharmacoeconomics 2002; 20 (4): 257–65
Sculpher M. Using economic evaluations to reduce the burden of asthma and chronic obstructive pulmonary disease. Pharmacoeconomics 2001; 19 Suppl. 2: 21–5
CEA Registry. League table of cost-utility analyses meeting panel criteria, with ratios converted to 1998 U.S. dollars [online]. Available from URL: http://www.hsph.harvard.edu/cearegistry/panelworthy.pdf [Accessed 2003 Aug 1]
Kelloway IS, Wyatt R, DeMarco J, et al. Effect of salmeterol on patients’ adherence to their prescribed refills for inhaled corticosteroids. Ann Allergy Asthma Immunol 2000; 84: 324–8
Spector S. Noncompliance with asthma therapy-are there solutions? J Asthma 2000; 37: 381–8
Milgrom H, Bender B, Ackerson L, et al. Noncompliance and treatment failure in children with asthma. J Allergy Clin Immunol 1996 Dec; 98 (6 Pt 1): 1051–7
Chapman KR, Walker L, Cluley S, et al. Improving patient compliance with asthma therapy. Respir Med 2000; 94: 2–9
Clark N, Jones P, Keller S, et al. Patient factors and compliance with asthma therapy. Respir Med 1999; 93: 856–62
Cochrane GM, Horne R, Chanex P. Compliance in asthma. Respir Med 1999; 93: 763–9
Pieters WR, Stallaert RALM, Prins J, et al. A study on the clinical equivalence and patient preference of fluticasone propionate 250 Ng twice daily via the Diskus/Accuhaler inhaler or the Diskhaler inhaler in adult asthmatic patients. J Asthma 1998; 35 (4): 337–45
Schlaeppi M, Edwards K, Fuller RW, et al. Patients perception of the Diskus inhaler: a comparison with the Turbuhaler inhaler. Br J Clin Pract 1996; 50: 14–9
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lyseng-Williamson, K.A., Plosker, G.L. Inhaled salmeterol/fluticasone propionate combination. Pharmacoeconomic 21, 951–989 (2003). https://doi.org/10.2165/00019053-200321130-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00019053-200321130-00004