Abstract
Objective
In hemodynamically unstable patients with spontaneous breathing activity, predicting volume responsiveness is a difficult challenge since the respiratory variation in arterial pressure cannot be used. Our objective was to test whether volume responsiveness can be predicted by the response of stroke volume measured with transthoracic echocardiography to passive leg raising in patients with spontaneous breathing activity. We also examined whether common echocardiographic indices of cardiac filling status are valuable to predict volume responsiveness in this category of patients.
Design and setting
Prospective study in the medical intensive care unit of a university hospital.
Patients
24 patients with spontaneously breathing activity considered for volume expansion.
Measurements
We measured the response of the echocardiographic stroke volume to passive leg raising and to saline infusion (500 ml over 15 min). The left ventricular end-diastolic area and the ratio of mitral inflow E wave velocity to early diastolic mitral annulus velocity (E/Ea) were also measured before and after saline infusion.
Results
A passive leg raising induced increase in stroke volume of 12.5% or more predicted an increase in stroke volume of 15% or more after volume expansion with a sensitivity of 77% and a specificity of 100%. Neither left ventricular end-diastolic area nor E/Ea predicted volume responsiveness.
Conclusions
In our critically ill patients with spontaneous breathing activity the response of echocardiographic stroke volume to passive leg raising was a good predictor of volume responsiveness. On the other hand, the common echocardiographic markers of cardiac filling status were not valuable for this purpose.
Similar content being viewed by others
Introduction
In mechanically ventilated patients who do not trigger the ventilator the response to volume expansion can be predicted by the respiratory variation in stroke volume or arterial pressure [1–4]. However, such heart-lung interaction indices fail to predict fluid responsiveness in ventilated patients who experience inspiratory efforts [5–7]. The response of the descending aortic blood flow to passive leg raising (PLR) has been proposed to predict volume responsiveness in mechanically ventilated patients with spontaneous breathing activity when monitored with an esophageal Doppler probe [5]. Transthoracic echocardiography (TTE) is increasingly used for noninvasive hemodynamic assessment of critically ill patients since high-quality images and Doppler signals are obtained with recent TTE equipment [8]. TTE provides clinicians with valuable information including stroke volume, left ventricular preload, and filling. The stroke volume can be easily obtained using the left ventricular outflow track Doppler method [9]. The indexed left ventricular end-diastolic area (LVEDAi) is considered a valuable indicator of left ventricular preload [10, 11]. The ratio of pulsed Doppler transmitral flow in early diastole to early diastolic mitral annulus velocity measured by tissue Doppler imaging (E/Ea) is considered the best estimate of left ventricular filling pressure [12, 13].
The aim of our study was to answer the question: can TTE be used as a tool for predicting volume responsiveness in critically ill patients who experience spontaneous respiratory movements whatever the presence of mechanical support? We first analyzed the predictive value of the TTE stroke volume response to PLR. We also analyzed the predictive value of the most commonly used static echocardiographic indicators of left ventricular filling, namely LVEDAi and E/Ea. We expected that the response of TTE stroke volume to PLR was a better predictor of volume responsiveness than the preinfusion values of left ventricular filling indices.
Patients and methods
Patients
We studied patients with spontaneous breathing activity for whom the attending physician decided to perform a fluid challenge because of the presence of at least one of the following clinical signs of inadequate global perfusion: mean arterial pressure (MAP) below 60 mmHg, oliguria (urine output less than 0.5 ml/kg per hour for more than 2 h), delayed capillary refill, mottled skin, and tachycardia (heart rate higher than 100/min). Patients were excluded if they had aortic valvulopathy, mitral insufficiency greater than grade 2, or mitral stenosis, and if cardiac echogenicity was not satisfactory. This observational study was approved by the Ethics Committee of the Société de Réanimation de Langue Française. Patients were informed that they participated in this study.
The study included 24 patients, 14 of whom were mechanically ventilated but experienced spontaneous breathing. Patients' characteristics are presented in Table 1. Three were ventilated with pressure support (inspiratory pressure level 18 ± 3 cmH2O, end-expiratory pressure 5 ± 0 cmH2O), and 11 were ventilated in the assist controlled-mode (tidal volume 464 ± 56 ml) with a significant inspiratory effort which was detected by the inspection of the airway pressure curve and the monitoring of the spontaneous respiratory rate. Ten patients were breathing spontaneously without any mechanical support. Twelve received vasoactive drugs (11 norepinephrine, 1 dobutamine). Six patients presented with atrial fibrillation but did not exhibit abrupt or marked changes in the ventricular rate. No patient was excluded because of poor quality TTE images.
Echocardiographic measurements
The echocardiographic examination was performed by the same operator (B.L.) using a transthoracic ultrasound device (EnVisor, Philips), equipped with the tissue Doppler imaging program and a phased array transducer of 2.5 MHz. Conventional echocardiography including M-mode, two-dimensional, and Doppler measurements was performed. Echocardiographic images were recorded together with the electrocardiogram. All measurements were recorded on paper at a speed of 100 mm/s and were stored digitally in the hardware for later playback and analysis. All measurements were evaluated by two physicians (B.L. and A.O.) and the average values were considered for the analyses.
Stroke volume
The stroke volume was calculated as the product of the velocity time integral of aortic blood flow (VTIAo) by the aortic valve area. Using the apical five-chamber view the VTIAo was computed from the area under the envelope of the pulsed-wave Doppler signal obtained at the level of the aortic annulus. The VTIAo value was averaged over five to ten consecutive measurements in sinus rhythm patients and over ten measurements in patients with atrial fibrillation. Using the parasternal long axis view the diameter of the aortic orifice was measured at the insertion of the aortic cusp and the aortic valve area was calculated (π diameter2/4). As the diameter of the aortic orifice is assumed to remain constant in a given patient, the diameter was measured once at baseline. The stroke volume index (SVi) was calculated as the ratio of stroke volume over body surface area. The cardiac output was calculated as the product of stroke volume by the heart rate.
Left ventricular end diastolic area
Using the short-axis, cross-sectional view the left ventricular end-diastolic area was measured by manual planimetry of the area circumscribed by the leading edge of the left ventricular endocardial border. The mean value of at least five consecutive measurements was calculated. The LVEDAi was calculated as the ratio of the averaged left ventricular end-diastolic area over body surface area.
Ratio of the transmitral flow in early diastole to the early diastolic mitral annulus velocity
Using the apical four-chamber view the early (E) peak diastolic velocity was measured by the pulsed-wave Doppler. The early (Ea) velocity of the lateral mitral annulus was measured by tissue Doppler imaging. The E/Ea ratio for the lateral mitral annulus was then calculated. The mean value of at least five consecutive measurements was considered for the analysis.
Left ventricular ejection fraction
We measured left ventricular ejection fraction (LVEF) using the biplane Simpson's method from the apical-two and four-chamber views.
Blood pressure measurements
Systolic arterial pressure (SAP) and MAP were measured either using an oscillometric cuff system at the brachial artery level or using an artery catheter when available.
Study design
SAP, MAP, heart rate, LVEF, VTIAo, and aortic valve area were measured at baseline while the patient was in the semirecumbent position (45 °). From this position an automatic bed elevation allowed to lift the lower limbs of the patient to a 45 ° angle while the patient's trunk was lowered from semirecumbent to supine position. The position of the Doppler probe was adjusted so as to obtain the best aortic flow signal. A second set of SAP, MAP, heart rate, and VTIAo measurements was collected during PLR at the moment when VTIAo plateaued at its highest value. The patient was then returned to his/her initial semirecumbent position. Measurements of SAP, MAP, heart rate, and VTIAo were performed once again. Measurements of LVEDAi and E/Ea were also obtained. Finally, measurements of SAP, MAP, heart rate, VTIAo, LVEDAi, and E/Ea were obtained after volume expansion, which was performed for 15 min with 500 ml saline. Since the aortic area was measured only at baseline, the value of SVi at each period was calculated as the product of the baseline aortic area by the VTIAo measured at each period. The ventilator settings and drugs were maintained at constant levels throughout the study period. All volume challenges were performed at the discretion of the attending physician according to the presence of one or more of the following criteria: MAP 60 mmHg or higher (n = 9), oliguria (n = 6), mottled skin (n = 7), and tachycardia (n = 10).
An increase in SVi of 15% or more after volume expansion defined a responder patient. According to this definition of fluid responsiveness, 13 patients were responders. These included seven who were intubated and three who had atrial fibrillation. The 11 nonresponders included seven who were intubated and three who had atrial fibrillation. baseline LVEF was similar in responders (50 ± 12%) and nonresponders (52 ± 13%). Before PLR the heart rate, SAP, MAP, VTIAo, and SVi did not differ between responders and nonresponders, and in neither responders nor nonresponders was there a difference between values before PLR or before volume expansion in any of the hemodynamic variables that were measured at both times (Table 2).
Statistical analysis
Results are expressed as mean ± SD. Hemodynamic variables were compared between responders and nonresponders before PLR and volume expansion using the nonparametric Mann–Whitney test. For the overall population and for each subgroup (responders and nonresponders) the nonparametric Wilcoxon rank sum test was used to assess the statistical significance of changes in hemodynamic parameters induced by PLR or by volume expansion and to compare the pre-PLR and preinfusion values of the variables measured at these two baseline periods (heart rate, SAP, MAP, SVi, VTIAo). The area under the receiver operating characteristic (ROC) curves (± SE) for PLR-induced changes in SVi (or in VTIAo), baseline (before volume expansion) LVEDAi and E/Ea were compared in all patients using the Hanley–McNeil test. Interobserver variability was assessed in ten randomly selected sets of measurements of VTIAo; LVEDAi and E/Ea and was calculated as the ratio (expressed as a percentage) of the difference between the values obtained by each observer (expressed as absolute value) divided by the mean of the two values. Each value (obtained by each observer) was the average of five to ten consecutive measurements. Intraobserver variability was calculated by a similar approach. Differences with a p value less than 0.05 were considered statistically significant. Statistical analyses were performed using Statview 5.0 software (Abacus Concepts, Berkeley Calif., USA) and Medcalc 8.1.0.0 software (Mariakerke, Belgium).
Results
Changes in VTIAo and SVi induced by PLR and by volume expansion
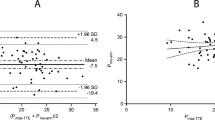
In all patients the highest plateau value of VTIAo recorded during PLR was obtained within the first 90 s following leg elevation. The proportional changes in VTIAo induced by PLR were correlated with the proportional changes in VTIAo induced by volume expansion (r = 0.83, p< 0.0001). The proportional changes in cardiac output induced by PLR were also correlated with the proportional changes in cardiac output induced by volume expansion (r = 0.79, p< 0.0001; Fig. 1). The PLR-induced changes in VTIAo or in SVi of 12.5% or more predicted fluid responsiveness with a sensitivity of 77% and a specificity of 100% (Fig. 2). Intubated and nonintubated patients did not differ. Among the three patients with false-negative findings (volume responders with a PLR-induced increase in VTIAo less than 12.5%) one was intubated and two nonintubated.
Individual values (open circles) and mean ± SD values (closed circles) of the passive leg raising (PLR) induced changes in VTIAo (velocity time integral of aortic blood flow), E/Ea [ratio of pulsed Doppler transmitral flow in early diastole (E) to the early diastolic mitral annulus velocity (Ea) measured by tissue Doppler imaging] before volume expansion (VE), and indexed left ventricular end-diastolic area (LVEDAi) before VE in responders (R, patients experiencing VE-induced increase in stroke volume ≥ 15%) and nonresponders (NR). Dotted line Best threshold value (+12.5%) of PLR-induced change in VTIAo that discriminates responders from nonresponders to VE
LVEDAi, E/Ea, and the effects of volume expansion
Before volume expansion LVEDAi and E/Ea did not differ between responders and nonresponders (Table 3, Fig. 2). The area under the ROC curve for PLR-induced changes in VTIAo (0.96 ± 0.04) was significantly greater than that for LVEDAi before volume expansion (0.58 ± 0.12) and that for E/Ea before volume expansion (0.65 ± 0.11;) (Fig. 3). For VTIAo measurements interobserver variability was 3.2 ± 2.5% and intraobserver variability 2.8 ± 2.2%. For LVEDAi measurements the interobserver variability was 6.5 ± 4.2% and intraobserver variability 5.8 ± 3.1%. For E/Ea measurements interobserver variability was 7.2 ± 5.3% and intraobserver variability 4.9 ± 4.5%. Finally, a fluid-induced increase in SVi of more than 10% (in 16 patients) was predicted by a PLR-induced increase in VTIAo greater than 8% with a sensitivity of 100% and a specificity of 100%.
Receiver operating characteristics curves comparing the ability of passive leg raising (PLR) induced changes in VTIAo (velocity time integral of aortic blood flow), E/Ea [ratio of pulsed Doppler transmitral flow in early diastole (E) to the early diastolic mitral annulus velocity (Ea) measured by tissue Doppler imaging] before volume expansion (VE), and indexed left ventricular end-diastolic area (LVEDAi) before VE to discriminate responders and nonresponders in the overall population. The area under the curve for PLR-induced changes in VTIAo was significantly greater than that for E/Ea before VE (difference 0.301, 95% confidence interval 0.077–0.524, p = 0.008) and for LVEDAi before VE (difference 0.374, 95% confidence interval 0.175–0.573, p = 0.0001). There was no difference between the area under the curve values for E/Ea before VE or for LVEDAi before VE
Discussion
The main results of our study performed in patients with spontaneous breathing activity are as follows: (a) a PLR-induced increase in VTIAo or in SVi of 12.5% or more predicted an increase in SVi of 15% or more after volume expansion with a sensitivity of 77% and a specificity of 100%, (b) the echocardiographic markers of filling status as LVEDAi and E/Ea did not accurately predict volume responsiveness.
The major strength of our study was to bring evidence that the response to volume expansion can be noninvasively predicted by a simple tool (PLR) in patients experiencing spontaneous respiratory movements. In such patients volume responsiveness is difficult to predict [1, 14] since heart-lung interaction indices such as stroke volume and arterial pulse pressure variations are not reliable for this purpose [5–7]. Importantly, this subgroup of patients represents the great majority of critically ill patients considered for volume expansion [3] including patients breathing spontaneously without any mechanical support and patients triggering their ventilator.
The PLR is able to induce a reversible increase in venous return from the legs to the thorax and then a reversible increase in preload of the right [15] and left ventricle [16]. Thus the PLR can be considered as a reversible self fluid challenge [17]. However, the effects of PLR on cardiac output are variable [5, 16, 18–20] depending upon the degree of leg elevation and the presence of cardiac preload reserve. Using pulmonary artery thermodilution Boulain et al. [19] found that the increase in stroke volume induced by PLR occurs only in patients who increase their stroke volume after a subsequent volume loading. Consequently PLR has been proposed to detect fluid responsiveness in critically ill patients [3, 17]. Recently we reported that PLR-induced changes in the descending aorta blood flow accurately predict volume responsiveness in patients monitored with an esophageal Doppler probe [5]. In our previous study a PLR increase in aortic blood flow of 10% or more predicted fluid responsiveness with a sensitivity of 97% and a specificity of 94% [5]. One of the major strengths of the present study was to find fairly consistent results by using a totally noninvasive device.
Importantly, the findings of the present study also demonstrate that the usual echocardiographic measures of cardiac filling, namely LVEDAi and E/Ea, are not reliable in predicting the response to volume expansion. The LVEDAi is considered a more valuable indicator of left ventricular preload than the pulmonary artery occlusion pressure (PAOP) [10], and LVEDAi has been shown to decrease during acute blood losses [21]. However, in mechanically ventilated patients LVEDAi appears to be of little value in predicting volume responsiveness [2, 22–24]. Pulsed Doppler analysis and tissue Doppler imaging are other approaches to assess cardiac filling. The E/Ea ratio is now considered as one of the best Doppler estimates of left ventricular filling pressure [12, 13, 25]. Its advantage is that Ea is assumed to be preload independent, thus allowing the effect of left ventricular relaxation on the E velocity to be corrected [25]. In addition, E/Ea is still reliable in patients with atrial fibrillation [26]. In critically ill patients the agreement between E/Ea and PAOP is only fair [27, 28]. In the present study the E/Ea value before volume expansion did not reliably predict volume responsiveness, and this finding was in accordance with the poor value of PAOP to predict volume responsiveness [1, 14]. In addition, in healthy volunteers E/Ea has been shown to be poorly correlated with PAOP during changes in preload [29], and it has been recently hypothesized that Ea varies with preload under conditions where left ventricular relaxation is normal [30, 31]. This may partly account for the absence of change in E/Ea with volume expansion in our patients.
There are at least three reasons for explaining the poor value of echocardiography indices of left ventricular filling to predict volume responsiveness. First, these parameters do not reflect the preload of the right ventricle, which is important to take into account when volume responsiveness is considered [3]. Second, none of these markers are accurate measures of left ventricular preload, which is conceptually considered as the left ventricular end-diastolic stress [32]. Third, a given value of ventricular preload can be associated with various degrees of ventricular preload reserve since the slope of the Frank–Starling curve (ventricular preload vs. stroke volume) highly depends on systolic cardiac function [32].
The limitations of our study must be discussed. We have learned from previous studies performed by our group [5, 19] and by others [33] that PLR results in transient hemodynamic effects. Thus we anticipated that we would not have enough time to perform a complete echocardiographic examination during PLR. Consequently we chose to focus on the responses of VTIAo to PLR, and this was both relevant with respect to our hypothesis and feasible within approx. 1 min. We measured stroke volume using the classical left ventricular outflow track Doppler method, which has been previously validated against the thermodilution technique [9] and is commonly used in critically ill patients [34], especially for predicting volume responsiveness [24, 35]. We defined the positive response to volume expansion as an increase in SVi of 15% or more with volume expansion. This cutoff value seems clinically relevant, and it was chosen by reference to previous studies [1, 2, 23–25, 36]. Six of our patients had atrial fibrillation with no abrupt, marked changes in ventricular rhythm. The distribution among responders (n = 3) and nonresponders (n = 3) was similar to that in the subgroup of patients with sinus rhythm. However, our findings cannot be extrapolated to patients experiencing abrupt and marked changes in the ventricular rate. It is known that the aortic area measured at the level of aortic annulus is unchanged during acute hemodynamic changes. Consequently, evaluating the response of VTIAo to PLR makes simpler the TTE detection of volume responsiveness and thus would enhance its clinical applicability. We obtained good quality imaging with transthoracic approach in all patients. This is now the general case in the intensive care units utilizing the new generations of TTE imaging equipments [8], although there are still particular patients with poor echogenicity in whom this technique cannot be reliably used.
Conclusion
Our study shows that the response of TTE stroke volume to PLR is a good predictor of volume responsiveness in patients with spontaneous breathing activity. Conversely, TTE static measures of cardiac preload were not found to be valuable for this purpose. Because predicting the response to volume expansion is a difficult challenge in patients with spontaneous breathing activity, we suggest that performing TTE during a simple test such as PLR may be useful. The response of VTIAo to PLR can predict the hemodynamic efficacy of fluid therapy, although it seems rather a marker of a positive response than a marker of a nonindication to fluid administration. Such findings should encourage clinicians to extend further the use of echocardiography as a first-line hemodynamic approach in patients with hemodynamic instability [37–39].
References
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, Richard C, Pinsky MR, Teboul JL (2000) Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med 162:134–138
Preisman S, Kogan S, Berkenstadt H, Perel A (2005) Predicting fluid responsiveness in patients undergoing cardiac surgery: functional haemodynamic parameters including the respiratory systolic variation test and static preload indicators. Br J Anaesth 95:746–755
Pinsky MR, Payen D (2005) Functional hemodynamic monitoring. Crit Care 9:566–572
Magder S (2004) Clinical usefulness of respiratory variations in arterial pressure. Am J Respir Crit Care Med 169:151–155
Monnet X, Rienzo M, Osman D, Anguel N, Richard C, Pinsky MR, Teboul JL (2006) Passive leg raising predicts fluid responsiveness in the critically ill. Crit Care Med 34:1402–1407
Heenen S, De Backer D, Vincent JL (2006) How can the response to volume expansion in patients with spontaneous respiratory movements be predicted? Crit Care 10:R102
Perner A, Faber T (2006) Stroke volume variation does not predict fluid responsiveness in patients with septic shock on pressure support ventilation. Acta Anaesthesiol Scand 50:1068–1077
Joseph MX, Disney PJ, Da Costa R, Hutchison SJ (2004) Transthoracic echocardiography to identify or exclude cardiac cause of shock. Chest 126:1592–1597
Huntsman LL, Stewart DK, Barnes SR, Franklin SB, Colocousis JS, Hessel EA (1983) Noninvasive Doppler determination of cardiac output in man. Clinical validation. Circulation 67:593–602
Thys DM, Hillel Z, Goldman ME, Mindich BP, Kaplan JA (1987) A comparison of hemodynamic indices derived by invasive monitoring and two-dimensional echocardiography. Anesthesiology 67:630–634
Coriat P, Vrillon M, Perel A, Baron JF, Le Bret F, Saada M, Viars P (1994) A comparison of systolic blood pressure variations and echocardiographic estimates of end-diastolic left ventricular size in patients after aortic surgery. Anesth Analg 78:46–53
Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quinones MA (1997) Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 30:1527–1533
Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, Tajik AJ (2000) Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures. A comparative simultaneous Doppler catheterization study. Circulation 102:1788–1794
Coudray A, Romand JA, Treggiari M, Bendjelid K (2005) Fluid responsiveness in spontaneously breathing patients: A review of indexes used in intensive care. Crit Care Med 33:2757–2762
Thomas M, Shillingford J (1965) The circulatory response to a standard postural change in ischaemic heart disease. Br Heart J 27:17–27
De Hert SG, Robert D, Cromheecke S, Michard F, Nijs J, Rodrigus IE (2006) Evaluation of left ventricular function in anesthetized patients using femoral artery dP/dt (max). J Cardiothorac Vasc Anesth 20:325–330
Teboul JL, Monnet X, Richard C (2005) Arterial pulse pressure variation during positive pressure ventilation and passive leg raising. In: Pinsky MR, Payen D (eds) Functional hemodynamic monitoring, 1st edn. Springer, Berlin Heidelberg New York, pp 331–343
Reich DL, Konstadt SN, Raissi S, Hubbard M, Thys DM (1989) Trendelenburg position and passive leg raising do not significantly improve cardiopulmonary performance in the anesthetized patient with coronary artery disease. Crit Care Med 17:313–317
Boulain T, Achard JM, Teboul JL, Richard C, Perrotin D, Ginies G (2002) Changes in BP induced by passive leg raising predict response to fluid loading in critically ill patients. Chest 121:1245–1252
Lafanechere A, Pene F, Goulenok C, Delahaye A, Mallet V, Choukroun G, Chiche J, Mira J, Cariou A (2006) Changes in aortic blood flow induced by passive leg raising predict fluid responsiveness in critically ill patients. Crit Care 10:R132
Cheung AT, Savino JS, Weiss SJ, Aukburg SJ, Berlin JA (1994) Echocardiographic and hemodynamic indexes of left ventricular preload in patients with normal and abnormal ventricular function. Anesthesiology 81:376–387
Lattik R, Couture P, Denault AY, Carrier M, Harel F, Taillefer J, Tardif JC (2002) Mitral Doppler indices are superior to two-dimensional echocardiographic and hemodynamic variables in predicting responsiveness of cardiac output to a rapid intravenous infusion of colloid. Anesth Analg 94:1092–1099
Tavernier B, Makhotine O, Lebuffe G, Dupont J, Scherpereel P (1998) Systolic pressure variation as a guide to fluid therapy in patients with sepsis induced hypotension. Anesthesiology 89:1313–1321
Feissel M, Michard F, Mangin I, Ruyer O, Faller JP, Teboul JL (2001) Respiratory changes in aortic blood velocity as an indicator of fluid responsiveness in ventilated patients with septic shock. Chest 119:867–873
Nagueh SF (1999) Noninvasive evaluation of hemodynamics by Doppler echocardiography. Curr Opin Cardiol 14:217–224
Sohn DW, Song JM, Zo JH, Chai IH, Kim HS, Chun HG, Kim HC (1999) Mitral annulus velocity in the evaluation of left ventricular diastolic function in atrial fibrillation. J Am Soc Echocardiogr 12:927–931
Bouhemad B, Nicolas-Robin A, Benois A, Lemaire S, Goarin JP, Rouby JJ (2003) Echocardiographic Doppler assessment of pulmonary capillary wedge pressure in surgical patients with postoperative circulatory shock and acute lung injury. Anesthesiology 98:1091–1100
Combes A, Arnoult F, Trouillet JL (2004) Tissue Doppler imaging estimation of pulmonary artery occlusion pressure in ICU patients. Intensive Care Med 30:75–81
Firstenberg MS, Levine BD, Garcia MJ, Greenberg NL, Cardon L, Morehead AJ, Zuckerman J, Thomas JD (2000) Relationship of echocardiographic indices to pulmonary capillary wedge pressures in healthy volunteers. J Am Coll Cardiol 36:1664–1669
Jacques DC, Pinsky MR, Severyn D, Gorcsan J 3rd (2004) Influence of alterations in loading on mitral annular velocity by tissue Doppler echocardiography and its associated ability to predict filling pressures. Chest 126:1910–1918
Firstenberg MS, Greenberg NL, Main ML, Drinko JK, Odabashian JA, Thomas JD, Garcia MJ (2001) Determinants of diastolic myocardial tissue Doppler velocities: influences of relaxation and preload. J Appl Physiol 90:299–307
Braunwald E, Sonnenblick EH, Ross J (1988) Mechanisms of cardiac contraction and relaxation. In: Braunwald E (ed) Heart disease. Saunders, Philadelphia, pp 383–425
Wong DH, Tremper KK, Zaccari J, Hajduczek J, Konchigeri HN, Hufstedler SM (1988) Acute cardiovascular response to passive leg raising. Crit Care Med 16:123–125
Poelaert JI (2001) Haemodynamic monitoring. Curr Opin Anaesthesiol 14:27–32
Slama M, Masson H, Teboul JL, Arnout ML, Susic D, Frohlich E, Andrejak M (2002) Respiratory variations of aortic VTI: a new index of hypovolemia and fluid responsiveness. Am J Physiol Heart Circ Physiol 283:H1729–H1733
De Backer D, Heenen S, Piagnerelli M, Koch M, Vincent JL (2005) Pulse pressure variations to predict fluid responsiveness: influence of tidal volume. Intensive Care Med 31:517–523
Cholley BP, Vieillard-Baron A, Mebazaa A (2006) Echocardiography in the ICU: time for widespread use! Intensive Care Med 32:9–10
Vignon P (2005) Hemodynamic assessment of critically ill patients using echocardiography Doppler. Curr Opin Crit Care 11:227–234
Vieillard-Baron A, Charron C, Chergui K, Peyrouset O, Jardin F (2006) Bedside echocardiographic evaluation of hemodynamics in sepsis: is a qualitative evaluation sufficient? Intensive Care Med 32:1547–1552
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-007-0645-8
Rights and permissions
About this article
Cite this article
Lamia, B., Ochagavia, A., Monnet, X. et al. Echocardiographic prediction of volume responsiveness in critically ill patients with spontaneously breathing activity. Intensive Care Med 33, 1125–1132 (2007). https://doi.org/10.1007/s00134-007-0646-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0646-7