Abstract
Background
Dyspnea is the most common symptom in patients with malignant pleural effusion (MPE). Treatment decisions are primarily based on the perception of dyspnea severity.
Aims
To study dyspnea perception following therapeutic thoracentesis using the visual analog scale (VAS) dyspnea score and modified Borg scale (MBS). To investigate whether patient reported outcome (PRO) measures can predict pleural re-interventions.
Patients and methods
Consecutive patients presenting with symptomatic MPE and planned for therapeutic thoracentesis were asked to complete MBS and VAS dyspnea scores (both at rest and during exercise) daily for 14 consecutive days. Physicians, unaware of the results of these PRO measures, decided on the necessity of a re-intervention, according to routine care. PRO measures were analyzed and correlated with performed re-interventions and the volume of removed fluid.
Results
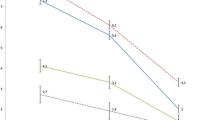
Forty-nine out of 64 consecutive patients returned the diaries. Twenty-eight patients (57 %) had a re-intervention within 30 days. Patients who required a re-intervention reported significantly higher MBS than patients who did not. The extent of increase in MBS during exercise was related to the need for re-intervention. Regarding the MBS during exercise, median time to maximal relief was 2 days. Re-intervention was required sooner when larger volumes were drained.
Conclusion
Patient reported outcomes are useful tools to assess treatment effect of therapeutic thoracentesis. Median time to maximal relief is 2 days. MBS rather than VAS dyspnea score appears to be more prognostic for repeat pleural drainage within 30 days.




Similar content being viewed by others
References
Light RW, Lee YC (2013) Textbook of pleural diseases, 2nd edn. Hodder Arnold, London, pp 41–43
Johnston WW (1985) The malignant pleural effusion. A review of cytopathologic diagnoses of 584 specimens from 472 consecutive patients. Cancer 56:905–909
Villena GV, Ferrer SJ, Hernandez BL, de Pablo GA, Perez RE, Rodriguez PF, Romero CS, Salvatierra VA, Valdes CL (2006) [Diagnosis and treatment of pleural effusion]. Arch Bronconeumol 42:349–372
Rodriguez-Panadero F, Borderas NF, Lopez MJ (1989) Pleural metastatic tumours and effusions. Frequency and pathogenic mechanisms in a post-mortem series. Eur Respir J 2:366–369
Chernow B, Sahn SA (1977) Carcinomatous involvement of the pleura: an analysis of 96 patients. Am J Med 63:695–702
Morgensztern D, Waqar S, Subramanian J, Trinkaus K, Govindan R (2012) Prognostic impact of malignant pleural effusion at presentation in patients with metastatic non-small cell lung cancer. J Thorac Oncol 7:1485–1489
Erasmus JJ, Patz EF Jr (1999) Treatment of malignant pleural effusions. Curr Opin Pulm Med 5:250–255
Roberts ME, Neville E, Berrisford RG, Antunes G, Ali NJ (2010) Management of a malignant pleural effusion: British thoracic society pleural disease guideline 2010. Thorax 65(Suppl 2):ii32–ii40
Shumway NM, Wilson RL, Howard RS, Parker JM, Eliasson AH (2008) Presence and treatment of air hunger in severely ill patients. Respir Med 102:27–31
Hareendran A, Leidy NK, Monz BU, Winnette R, Becker K, Mahler DA (2012) Proposing a standardized method for evaluating patient report of the intensity of dyspnea during exercise testing in COPD. Int J Chron Obstruct Pulmon Dis 7:345–355
Martinez JA, Straccia L, Sobrani E, Silva GA, Vianna EO, Filho JT (2000) Dyspnea scales in the assessment of illiterate patients with chronic obstructive pulmonary disease. Am J Med Sci 320:240–243
Bausewein C, Farquhar M, Booth S, Gysels M, Higginson IJ (2007) Measurement of breathlessness in advanced disease: a systematic review. Respir Med 101:399–410
Davies HE, Mishra EK, Kahan BC, Wrightson JM, Stanton AE, Guhan A, Davies CW, Grayez J, Harrison R, Prasad A, Crosthwaite N, Lee YC, Davies RJ, Miller RF, Rahman NM (2012) Effect of an indwelling pleural catheter vs chest tube and talc pleurodesis for relieving dyspnea in patients with malignant pleural effusion: the TIME2 randomized controlled trial. JAMA 307:2383–2389
Putnam JB Jr, Light RW, Rodriguez RM, Ponn R, Olak J, Pollak JS, Lee RB, Payne DK, Graeber G, Kovitz KL (1999) A randomized comparison of indwelling pleural catheter and doxycycline pleurodesis in the management of malignant pleural effusions. Cancer 86:1992–1999
Marcondes BF, Vargas F, Paschoal FH, Cartaxo AM, Teixeira LR, Genofre EH, Onishi R, Skomro R, Lorenzi-Filho G (2012) Sleep in patients with large pleural effusion: impact of thoracentesis. Sleep Breath 16:483–489
Cartaxo AM, Vargas FS, Salge JM, Marcondes BF, Genofre EH, Antonangelo L, Marchi E, Teixeira LR (2011) Improvements in the 6-min walk test and spirometry following thoracentesis for symptomatic pleural effusions. Chest 139:1424–1429
Wilson RC, Jones PW (1989) A comparison of the visual analogue scale and modified Borg scale for the measurement of dyspnoea during exercise. Clin Sci (Lond) 76:277–282
Barbera L, Taylor C, Dudgeon D (2010) Why do patients with cancer visit the emergency department near the end of life? CMAJ 182:563–568
Wallace EM, Walsh J, Conroy M, Cooney MC, Twomey F (2012) Why do palliative care patients present to the emergency department? Avoidable or unavoidable? Am J Hosp Palliat Care 30(3):253–256
Morris NR, Sabapathy S, Adams L, Kingsley RA, Schneider DA, Stulbarg MS (2007) Verbal numerical scales are as reliable and sensitive as visual analog scales for rating dyspnea in young and older subjects. Respir Physiol Neurobiol 157:360–365
von LA, Dahme B (2005) Differentiation between the sensory and affective dimension of dyspnea during resistive load breathing in normal subjects. Chest 128:3345–3349
von LA, Ambruzsova R, Nordmeyer S, Jeske N, Dahme B (2006) Sensory and affective aspects of dyspnea contribute differentially to the Borg scale's measurement of dyspnea. Respiration 73:762–768
Acknowledgments
We are grateful to our colleagues at the data center of the Dutch Society of Pulmonologists for analyzing the patient reported outcome measures. We would like to acknowledge Prof. Dr. Aaronson who reviewed the draft manuscript and provided us with valuable advices. The Netherlands Cancer Institute receives a research grant funding from the Dutch Cancer Society and Nuts-OHRA for the treatment of malignant pleural effusion.
Conflict of Interest
None of the authors reported any conflicting interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 53 kb)
Rights and permissions
About this article
Cite this article
Boshuizen, R.C., Vincent, A.D. & van den Heuvel, M.M. Comparison of modified Borg scale and visual analog scale dyspnea scores in predicting re-intervention after drainage of malignant pleural effusion. Support Care Cancer 21, 3109–3116 (2013). https://doi.org/10.1007/s00520-013-1895-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-1895-3