Abstract
Narrow Band Imaging (NBI) videobronchoscopy is a new technique for visualization of microvascular changes in bronchial mucosa. The primary aim of this study was to evaluate relation between vascular patterns visualized by NBI and histology of lung cancer. We prospectively evaluated 65 patients with suspected lung cancer scheduled for bronchoscopy. NBI followed conventional WL videobronchoscopy. After identification of endoscopically visible tumor, NBI was used to determine predominant type of pathological vascular pattern (dotted, tortuous, abrupt-ending blood vessels—Shibuya descriptors). All the lesions were biopsied and histologically confirmed. There were 81.5 % male and 18.5 % female patients evaluated in the study. Lung cancer was confirmed in all patients; 63.1 % were diagnosed with squamous cell lung cancer (SCC), 24.6 % had adenocarcinoma, 9.2 % had small-cell (SCLC) and 3.1 % large-cell lung cancer (LC). Dotted blood vessels were significantly (p < 0.000) associated with adenocarcinoma, identified in 68.4 % adenocarcinoma and 31.6 % SCC. Tortuous blood vessels were identified in 72 % SCC, 8 % adenocarcinoma, 12 % SCLC and 8 % of LC. Tortuous blood vessels were significantly (p < 0.000) associated with SCC. Abrupt-ending vessels were identified in 81 % SCC, 14.3 % SCLC and 4.8 % adenocarcinoma and were significantly associated (p < 0.000) with SCC. Dotted visual pattern of blood vessels identified during NBI videobronchoscopy is highly suggesting adenocarcinoma histology of lung cancer. Tortuous and abrupt-ending blood vessels visualized under NBI videobronchoscopy significantly suggest squamous cell histology of lung cancer. Large-scale studies should be designed in order to determine true relation between visual appearance and histology in lung cancer.
Similar content being viewed by others
Introduction
Narrow band imaging videobronchoscopy is one of the newest bronchoscopic imaging tools recently introduced in the clinical practice. This technique is designed for detection of pathologically altered submucosal and mucosal microvascular patterns. NBI creates enhanced images of the blood vessels in the surface layers of the mucosa and reveals vascular patterns on mucosal membranes when the tissue is irradiated with the two narrow wave bands of light [1–4]. One of the most explored NBI videobronchoscopy systems consists of NBI videobronchoscope and EVIS EXERA II (Olympus Co., Tokyo, Japan) videoendoscopy system. The NBI system uses blue narrow band, with the wavelength ranging from 390 to 445 nm, for imaging the capillaries of the surface mucosal layer. Green narrow band (wavelength from 530 to 550 nm) is used to visualize thick blood vessels inside the membranes [5–9]. This kind of approach enables better contrast on the mucosal surface, reduces examination time and eliminates futile biopsies. Integration of magnifying videobronchoscopy and narrow band imaging technology resulted in construction of first conventional NBI videobronchoscopy systems; however, due to high cost of the equipment and lack of experience, the use of the system is limited to high-volume research centers. NBI showed to be more efficient in detection of precancerous lesions, especially angiogenic squamous dyplasia (ASD), than the white light videobronchoscopy alone. Sharp learning curve makes this technology particularly suitable for inexperienced bronchoscopists because it enables better visualization of the bronchial mucosa and differentiations between malignant and non-malignant tissue [10–13].
NBI videobronchoscopy was so far evaluated as a tool for detection of premalignant bronchial lesions and as a tool that increases sensitivity of autofluorescence videobronchoscopy. In recent publications, NBI videobronchoscopy was found to be useful for endoscopic assessment of lung cancer extension with potential influence on therapeutic strategy [14–18].
Shibuya published the cornerstone studies for introduction of NBI videobronchoscopy in respiratory endoscopy and lung cancer diagnostics [14–16]. In these studies, NBI and magnification videobronchoscopy were used to investigate subepithelial patterns in bronchial dysplasia using a high-magnification videobronchoscope. First published trial was designed to investigate the value of magnification videobronchoscopy in detection of bronchial dysplasia of places with abnormal fluorescence. Vascular patterns described as dotted, tortuous and abrupt-ending micro-capillaries were identified as pathological. These patterns were most often identified in pathological samples of lung cancer. Later on, dotted, tortuous and abrupt-ending capillary grids identified on NBI videobronchoscopy became known as Shibuya’s descriptors and started to be widely used by bronchoscopists as pathological findings [9]. Usually, all three patterns are more or less present in endobronchial malignant lesions observed by the bronchoscopist. However, thorough observation confirms predominance of one sole pattern most spread throughout the observed tumor. In this study, we used consensus between two or three bronchoscopists in order to determine predominant vascular pattern in observed lesion.
The major aim of this study was to investigate association between certain pattern of pathological vascular capillary grid and histology of lung cancer. We hypothesized that there might be significant relations between dotted, tortuous and abrupt-ending type of pathological vascularization and histological types of lung cancer. Detection of various types of pathological vascular grids and their relation to specific histology of lung cancer could significantly improve investigation of angiogenesis during multi-step carcinogenesis in evolution of lung cancer.
Patients and methods
The study was a prospective, non-randomized trial, conducted at a dedicated respiratory endoscopy unit of a university teaching clinic at the Institute for Pulmonary Diseases of Vojvodina in Serbia in the period from Jun 2011 to December 2011. It was approved by the institutional review and ethics board. All of the patients who decided to participate in the study were informed about the procedure, potential benefits and the risks, and all of them had signed institutional informed consent form. All of the patients screened for the enrollment were previously scheduled for routine bronchoscopy due to high probability of lung cancer.
Inclusion criteria
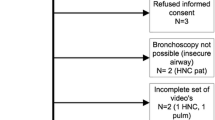
Inclusion criteria for enrollment in the study were age over 18 years, radiological suspicion for lung cancer, surveillance of patients after curative lung cancer surgery and evaluation of known lung cancer. Exclusion criteria were refusal to participate in the study, Eastern Cooperative Oncology Group performance status (ECOG) ≥3, recent myocardial infarction, unresolved coagulopathies, unstable angina pectoris, chronic heart failure New York Heart Association (NYHA) ≥3, uncontrolled arrhythmia or hypertension and allergy to anesthetics. Prior to the enrollment in the study, all patients must have had chest X-ray or CT scan the thorax, spirometry and body pletismography, blood gas analysis, complete blood count and blood biochemistry. Seventy eight patients were screened for the study, 65 of them met all the inclusion criteria, not having any exclusion.
Technique and design
Bronchoscopy was performed in a dedicated respiratory endoscopy unit by bronchoscopists experienced in the use of NBI. All procedures were performed in analgosedation. The routine vital parameters were monitored: non-invasive arterial blood pressure, oxygen saturation on pulls oximetry and ECG for cardiac rhythm. Brochoscopic equipment used in the study was NBI videobronchoscope BF-1T180 and BF-1TQ180 (Olympus Corporation, Tokyo, Japan), and video processor units EVIS LUCERA SPECTRUM (CV-260SL) and EXERA II (Olympus Corporation, Tokyo). Videobronchoscopy image was presented at a 19-inch LCD monitor OEV-191. The examination of the tracheobronhial tree started with WLB. NBI followed WLB videobronchoscopy. Once the pathologic sites were identified, targeted biopsies were performed in order to obtain material for pathological examination. Pathological vascular patterns were determined by Shibuya descriptors. Dotted, tortuous and abrupt-ending blood vessels were regarded as pathological. In order to establish predominance of one type of pathological vascularization an agreement between two bronchoscopists had to be reached. If the two could not agree on the predominance, a third bronchoscopist reviewed the video taken during bronchoscopy and decided which type of pathologic vascular pattern is predominant. A dedicated lung pathologist evaluated the biopsy specimens, blinded to bronchoscopic findings, in order to establish histological type of lung cancer.
Statistical analysis
Descriptive statistics were generated for all study variables, including mean and standard deviation (SD) for continuous variables and relative frequencies for categorical variables. One sample Kolmogorov–Smirnov test was performed for testing the goodness of fit with the normal distribution. Pearson chi Square was used to compare the diagnostic sensitivity and specificity, and statistically significant differences between categorical variables. All statistical analyses were performed with SPSS for Windows version 15.0 (SPSS Inc., Chicago, IL, USA).
Results
There were 65 patients enrolled in the study, 53 (81.5 %) males and 12 (18.5 %) females. Mean age of the patients was 55.67 ± 9.7 years. Majority of the patients were current smokers, 62%, 22 % were former smokers and 16 % were non-smokers. All patients were diagnosed with lung cancer, 41 (63.1 %) with squamous cell lung cancer (SCC) and 16 (24.6 %) with adenocarcinoma. There were 6 (9.2 %) patients with small-cell lung cancer and 2 (3.1 %) with large-cell lung cancer. Eight patients (12.3 %) were with Eastern Cooperative Oncology Group (ECOG) performance status 0, ECOG 1 performance status was present in 50 (76.9 %) of the patients, while ECOG 2 was observed in 7 (10.8 %) patients. There was no patients in stage IA, 3 (4.6 %) patients were diagnosed in stage IB, 2 (3.1 %) in stage IIA. Ten patients (15.4 %) were diagnosed in stage IIB, 19 (29.2 %) patients were in stage IIIA. Advanced stage lung cancer IIIB was diagnosed in 19 (29.2 %) patients and metastatic disease, and stage IV was diagnosed in 12 (18.5 %) patients.
Dotted vascular pattern was observed in 6 (31.6 %) patients with squamous cell lung cancer, and in 13 (68.4 %) patients with adenocarcinoma. This pattern was not observed in patients with small-cell lung cancer or large-cell lung cancer. Tortuous blood vessels were identified as predominant type of pathological vascularization in 18 (72 %) patients with squamous cell lung cancer, in 2 (8 %) patients with adenocarcinoma and 2 (8 %) patients with large-cell lung cancer. This type of vascular pattern was also observed in 3 (12 %) patients with small-cell lung cancer. Abrupt-ending blood vessels were most predominant type of pathological blood vessels in 17 (81 %) patients with squamous cell lung cancer, 16 (24.6 %) patients with adenocarcinoma and 6 (9.2 %) patients with small-cell lung cancer. Relationship between histological types of lung cancer and appearance of pathological vascular pattern is given in Table 1.
Dotted blood vessels were found to be significantly (p < 0.0001) related to adenocarcinoma histology. Tortuous and abrupt-ending pathological vascular grid was found to be significantly (p < 0.0001) related to squamous histology of lung cancer. There was no significant relation between visual appearance of pathological vascular grid and small-cell or large-cell lung cancer histology (Figs. 1, 2, 3, 4, 5, 6).
Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of dotted vascular pattern in diagnosis of adenocarcinoma were 0.821 (95 % CI 0.536–0.950), 0.877 (95 % CI 0.745–0.949), 0.684 (95 % CI 0.434–0.864) and 0.934 (95 % CI 0.810–0.983), respectively. Positive likelihood ratio (pLR) was 6.63, while negative likelihood ratio (nLR) was 0.21. Sensitivity, specificity, PPV and NPV of tortuous pathological pattern in diagnosis of squamous cell lung cancer (SCC) were 0.439 (95 % CI 0.288–0.601), 0.708 (95 % CI 0.487–0.865), 0.720 (0.504–0.871) and 0.425 (95 % CI 0.274–0.589), respectively. Positive likelihood ratio was 1.5, while nLR was 0.79. Sensitivity of abrupt-ending visual vascularization pattern in diagnosis of SCC was 0.414 (95 % CI 0.267–0.578), and specificity was 0.833 (95 % CI 0.618–0.945). Positive and negative predictive values were 0.809 (95 % CI 0.574–0.937) and 0.454 (95 % CI 0.306–0.610), respectively. Positive likelihood ratio was 2.48, while negative likelihood ratio was 0.70. Additional information on sensitivity, specificity, PPV, NPV and likelihood ratios are presented in Table 2.
Discussion
The primary aim of this study was to investigate relationship between visual appearance of pathological vascular grid under NBI videobronchoscopy and histology of lung cancer. Several clinical trials investigated potential role of NBI videobronchoscopy in detection of lung cancer and precancerous lesions. In one of the cornerstone studies, Shibuya [15] investigated role of high-magnification bronchovideoscopy in combination with narrow band imaging in detection of capillary loops of angiogenic squamous dysplasia (ASD) in heavy smokers at high risk for lung cancer. The investigation was carried out in relation to bronchial vascular patterns with abnormal mucosal fluorescence in heavy smokers. Forty eight patients with sputum cytology specimens suspicious or positive for malignancy were enrolled in the study. Similar enrollment pattern was used for out study; only we enrolled patients with high radiological probability for central lung cancer. Shibuya used several NBI filters with different wavelength ranges: NBI B1 filter (400–430 nm), NBI B2 filter (420–470 nm) and NBI G filter (560–590 nm). In our study, we used standard NBI equipment with two bandwidths of light: blue light 390–445 nm that is absorbed by superficial capillaries and green light 530–550 nm that is absorbed by thicker blood vessels underneath of mucosal capillaries. In Shibuya’s study, the microvessels, vascular networks of various grades and dotted vessels in ASD tissues were clearly observed in NBI-B1 images, the range which corresponds with blue light bandwidth in conventional NBI videobronchoscopy. The authors found significant association between the frequency of dotted vessels by NBI-B1 imaging and tissues confirmed as ASD pathologically (p = 0.002). In our study, significant association was found in the frequency of dotted vessels and adenocarcinoma histology (p < 0.0001), and between frequency of tortuous and abrupt-ending vessels and squamous histology (p < 0.0001). Shibuya and coauthors concluded that NBI may enable discrimination between ASD and other precancerous bronchial lesions. Similar conclusion ensues from our study, in which we confirmed that NBI could facilitate discrimination between adenocarcinoma and squamous histology. In most recent study published by Shibuya [16], authors investigated ability of NBI to detect blood vessel structures in squamous cell lung cancer (SCC) and squamous dysplasia. Authors found increased vessel growth and complex networks of tortuous vessels in squamous dysplasia. Some dotted vessels, increased vessel growth and complex networks of tortuous vessels were identified in ASD. Several dotted vessels and spiral or screw type tumor vessels were most often in squamous cell lung cancer. Results obtained from our study are completely comparable to Shibuya’s data. In our study, dotted vessels were confirmed to be predominant in only six patients (31.6 %) with squamous cell lung cancer. Most often in patients with SCC, we identified abrupt-ending vessels, present in 81 % of SCC patients while tortuous blood vessels were identified to be predominant in 72 % of patients. On the other hand, dotted vessels were present in 68.4 % of patients with adenocarcinoma, and there was significant association (p < 0.0001) between dotted vessels and adenocarcinoma.
Visual appearance of pathological microvascular networks may provide very important information about malignant potential of neoplastic lesions or disease severity in premalignant lesions. Detection of predominant vascular pattern along with exact measuring of vessel area ratio, vessel length ratio and vessel area to length ratio may contribute better differentiation between malignant and non-malignant bronchial lesions. Data from Yamada’s study [17] confirmed that NBI yields clear images of subepithelial microvessels in large airways of patients without abnormality in large airway mucosa. One of the pitfalls of NBI examination is high frequency of “background noise;” complex blood vessel networks which do not show dotted, tortuous and abrupt-ending pattern, but sometimes might be confusing. Major factor in avoiding this pitfall is experience of the bronchoscopist, but addition of software analysis and calculation of above-mentioned ratios might quantify the differences between pathological and normal blood vessels. Such software was already prototyped (SolemioEndoProStudy, Olympus Medical Systems, Tokyo, Japan) and used in clinical trial setting [17–23]. High-magnification videobronchoscopy, an integral part of conventional NBI system, was already used for investigation of subepithelial vascular patterns in bronchial dysplasia. The system was investigated in bronchial mucosa of patients with abnormal mucosal fluorescence by Shibuya and associates [14]. Vascular networks with increased vessel growth and complex networks of tortuous vessels of various sizes were observed in 15 of 21 abnormal fluorescence sites in dysplasia specimens. Significant difference was found between bronchitis and dysplasia specimens (p < 0.001). Mean vascular area ratios between normal bronchial mucosa, bronchitis and dysplasia were significantly different.
Dotted, tortuous and abrupt-ending visual appearance of subepithelial vascular network observed under NBI examination in lung cancer was used in majority of clinical trials that evaluated utility of this technique. Miyazu [18] investigated clinical utility of NBI for centrally located lesions in the lung using visual identification similar to Shibuya descriptors. Authors found intraepithelial capillary papillary loops (IPCL) in 30 of 38 squamous lung cancers. Sensitivity, specificity, PPV and NPV of IPCL in diagnosis of squamous cell lung cancer were 79, 97, 94 and 91 %, respectively. Results from our trial are in consistency with data obtained from Miyazu’s trial, except for slightly lower sensitivity. Sensitivity of tortuous vessels appearance for SCC in our trial was 43.9 % and sensitivity of abrupt-ending pattern for SCC histology was 41.4 %. Specificity for SCC histology in our trial was higher than sensitivity, 70.8 % for tortuous pattern and 83.3 % for abrupt-ending pattern. In Miyazu’s trial, cobblestone appearance (dotted vessels) were found in 11 of 15 (73.3 %) patients with adenocarcinoma; in our study, same pathological pattern was observed in 68.4 % of patients. Sensitivity, specificity, PPV and NPV of cobblestone appearance for adenocarcinoma in Miyazu’s study were 73, 96, 73 and 96 %, respectively. In our trial, corresponding values for sensitivity, specificity, PPV and NPV of dotted vascular pattern in adenocarcinoma was 81.2, 87.7, 68.4 and 93.4 %.
Narrow band imaging (NBI) videobronchoscopy demonstrated high sensitivity and specificity in detection of premalignant lesions and invasive lung cancer. This technique showed superiority over autofluorescence videobronchoscopy in detection of premalignant lesions, although much more large-scale clinical trials are necessary to confirm that superiority. Further investigation of pathological vascular patterns visualized by NBI videobronchoscopy end their relation to type and severity of premalignant lesions could provide significant insight into neoangiogenesis within carcinogenesis of bronchial cancers [19–23].
Conclusion
This study confirmed significant association between dotted pathological blood vessel pattern visualized by NBI videobronchoscopy and adenocarcinoma of the lung. Dotted pattern demonstrated high sensitivity and specificity in detection of lung cancer. Tortuous and abrupt-ending pathological capillary grid within bronchial mucosa showed significant association with squamous cell lung cancer. High specificity of this pattern suggests that during visual examination, bronchoscopist might presume squamous histology of lung cancer. Visual examination of bronchial mucosa under NBI can never substitute pathological examination; however, it can guide bronchoscopist to obtain sufficient amount of specific tissue. Lung cancer tissue obtained during bronchoscopy becomes more and more valuable due to the need for extensive genetic testing, especially in adenocarcinoma of the lung. Quick orientation by visual appearance of the lesion during bronchoscopy might result in acquisition of sufficient quantity of tissue for future molecular examination. Significant experience by the bronchoscopist is needed in order to establish which type of vascularization is predominant.
References
Colt HG, Murgu SD. Interventional bronchoscopy from bench to bedside: new techniques for early lung cancer detection. Clin Chest Med. 2010;31(1):29–37.
Gono K, Obi T, Yamaguchi M, et al. Appearance of enhanced tissue features in narrow-band endoscopic imaging. J Biomed Opt. 2004;9(3):568–77.
Yarmus L, Feller-Kopman D. Bronchoscopes of the twenty-first century. Clin Chest Med. 2010;31(1):19–27.
Yasufuku K. Early diagnosis of lung cancer. Clin Chest Med. 2010;31(1):39–47.
Herth F. Playing with the wavelengths: endoscopic early lung cancer detection. Lung Cancer. 2010;69(2):131–2.
Zaric B, Perin B. The use of narrow band imaging bronchoscopy in detection of lung cancer. Expert Rev Med Devices. 2010;7(3):395–406.
Miyazu Y, Ishida A, Nakamura M, et al. Possible clinical applications of high magnification bronchoscopy combined with narrow band imaging. Chest. 2006;130(4):146s.
Yamada G, Kitamura Y, Kitada J, Yamada Y, Takahashi M, Fujii M, Takahashi H. Increased microcirculation in subepithelial invasion of lung cancer. Intern Med. 2011;50(8):839–43.
Herth FJF, Eberhardt R, Anantham D, Gompelmann D, Zakaria MW, Ernst A. Narrow-band imaging bronchoscopy increases the specificity of bronchoscopic early lung cancer detection. J Thorac Oncol. 2009;4:1060–5.
Herth F, Eberhardt R, Ernst A. Narrow band imagining (NBI) for early lung cancer detection. Chest. 2006;130(4):146s.
Zaric B, Perin B, Becker HD, Herth FJ, Eberhardt R, Jovanovic S, Orlic T, Panjkovic M, Zvezdin B, Jovelic A, Bijelovic M, Jurisic V, Antonic M. Combination of narrow band imaging (NBI) and autofluorescence imaging (AFI) videobronchoscopy in endoscopic assessment of lung cancer extension. Med Oncol. 2012;29(3):1638–42.
Vincent BD, Fraig M, Silvestri GA. A pilot study of narrow-band imaging compared to white light bronchoscopy for evaluation of normal airways and premalignant and malignant airways disease. Chest. 2007;131:1794–9.
Park JK, Jo YS, Jang S, Park YS, Choi CM. Clinical benefits of narrow band imaging bronchoscopy in central lung cancer. Tuberc Respir Dis. 2010;68(1):16–21.
Shibuya K, Hoshino H, Chiyo M, Yasufuku K, Iizasa T, Saitoh Y, et al. Subepithelial vascular patterns in bronchial dysplasias using a high magnification bronchovideoscope. Thorax. 2002;57(10):902–7.
Shibuya K, Hoshino H, Chiyo M, Iyoda A, Yoshida S, Sekine Y, et al. High magnification bronchovideoscopy combined with narrow band imaging could detect capillary loops of angiogenic squamous dysplasia in heavy smokers at high risk for lung cancer. Thorax. 2003;58:989–95.
Shibuya K, Nakajima T, Fujiwara T, Chiyo M, Hoshino H, Moriya Y, et al. Narrow band imaging with high-resolution bronchovideoscopy: a new approach for visualizing angiogenesis in squamous cell carcinoma of the lung. Lung Cancer. 2010;69(2):194–202.
Yamada G, Shijubo N, Kitada J, Takahashi M, Otsuka M, Fujii M, et al. Narrow band imaging yields clear images of subepithelial microvessels in large airways in combination with high magnification bronchovideoscopy. J Bronchol. 2007;14:75–8.
Miyazu Y, Ishida A, Nakamura M, et al. Clinical utility of narrow band imaging for centrally located lesions in the lung. Chest. 2007;132(4):516s.
Zaric B, Perin B, Jovelic A, Stojanovic G, Ilic MD, Andrijevic I, et al. Influence of Narrow Band Imaging (NBI) Videobronchoscopy on the Assessment of Central Lung Cancer Extension and Therapeutic Decision. Cancer Invest. 2009;27:918–23.
Zaric B, Becker HD, Perin B, Jovelic A, Stojanovic G, Ilic MD, et al. Narrow band imaging (NBI) videobronchoscopy improves assessment of lung cancer extension and influences therapeutic strategy. Jpn J Clin Oncol. 2009;39:657–63.
Yasufuku K, Shibuya K, Fujisawa T. Narrow band imaging in the airway: where do we stand? J Bronchol. 2007;14(2):71–2.
Irani S, Thuer I, Seifert B, Speich R, Boehler A. Endoscopic narrow-band imaging-quantitative assessment of airway vascularity after lung transplantation. J Biomed Opt. 2009;14(1):014010.
East JE, Tan EK, Bergman JJ, Saunders BP, Tekkis PP. Meta-analysis: narrow band imaging for lesion characterization in the colon, oesophagus, duodenal ampulla and lung. Aliment Pharmacol Ther. 2008;28(7):854–67.
Acknowledgments
The study was supported by the grant of the Serbian Ministry for Science and Technology, grant number 175056.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zaric, B., Perin, B., Stojsic, V. et al. Relation between vascular patterns visualized by narrow band imaging (NBI) videobronchoscopy and histological type of lung cancer. Med Oncol 30, 374 (2013). https://doi.org/10.1007/s12032-012-0374-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-012-0374-x